One size fits all rarely works for clothing, and it turns out, it doesn’t work for prescription drug coverage either.
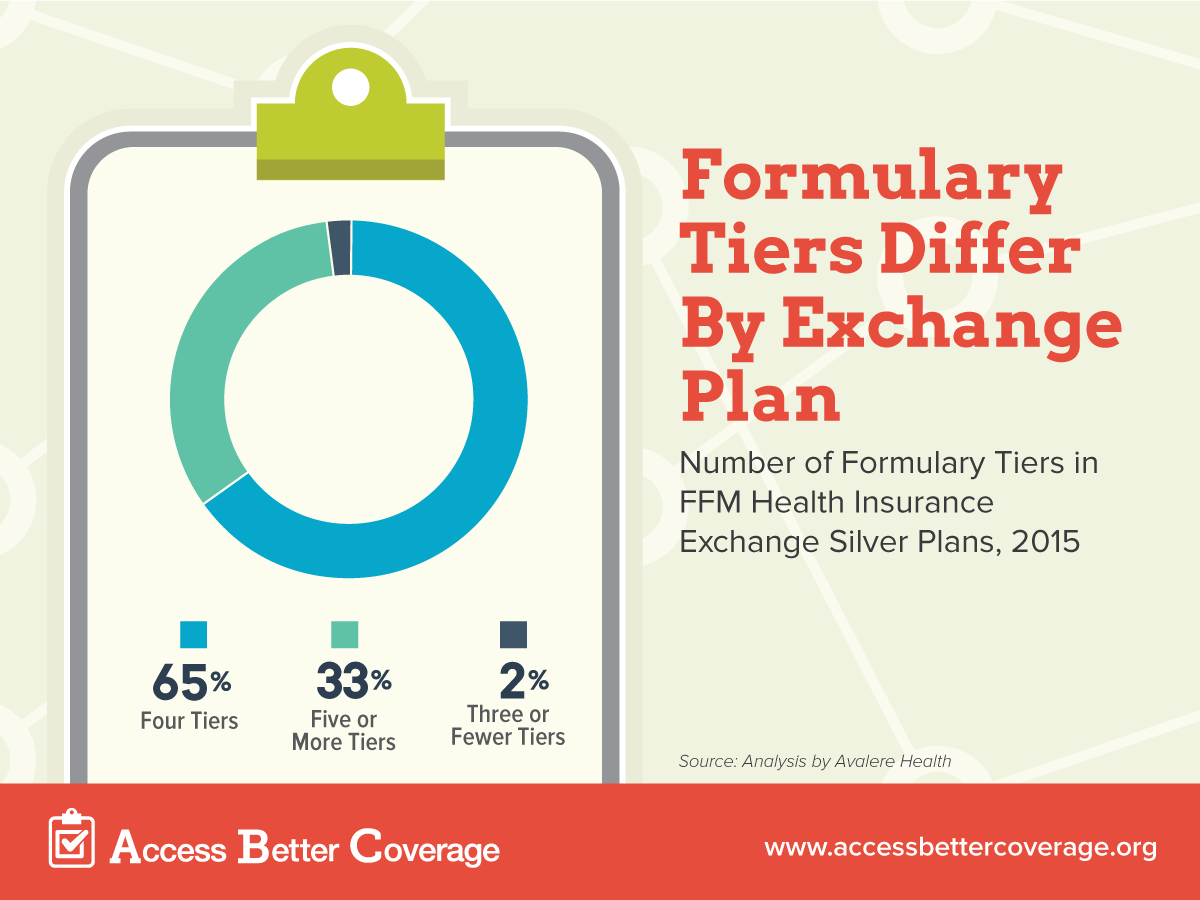
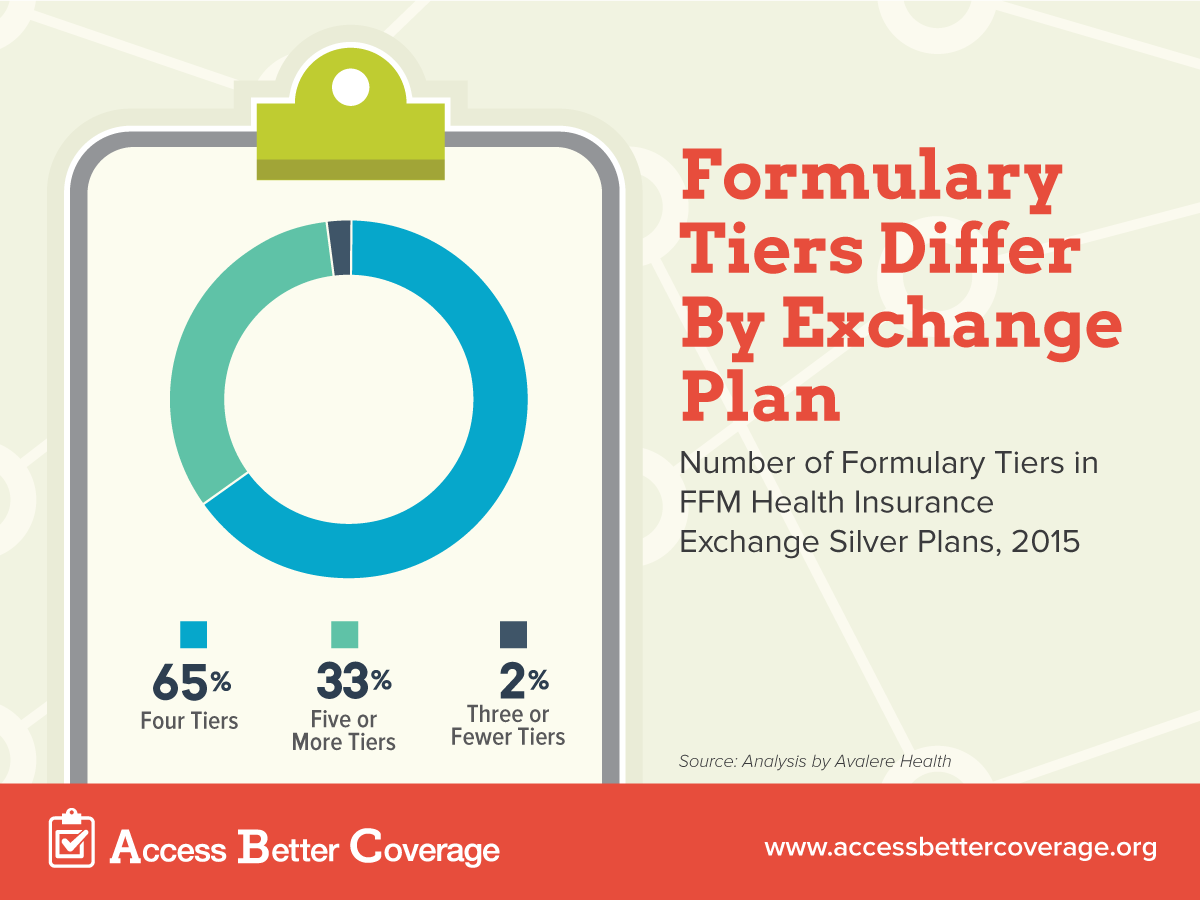
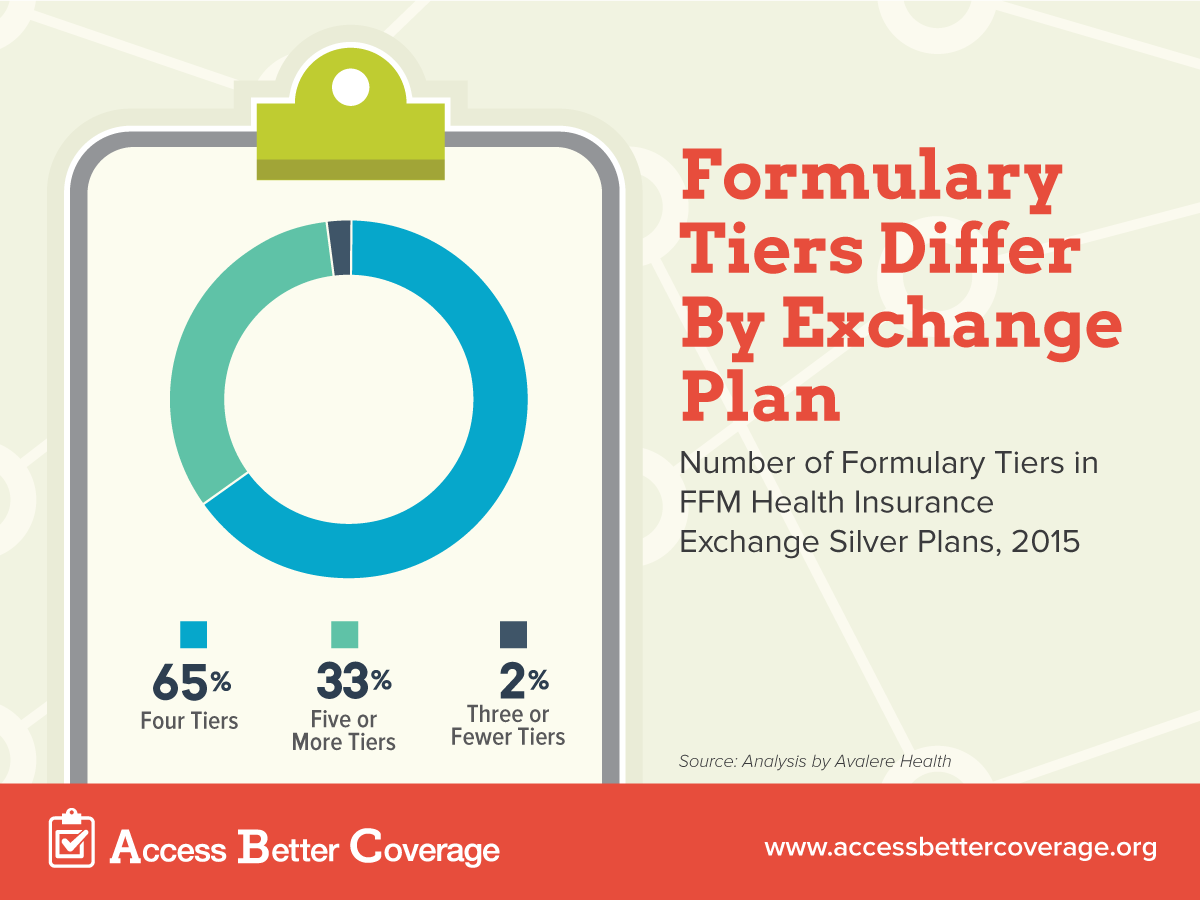
Health insurance plans cover prescription drugs through formularies, which list the medicines a plan covers (Watch our video for more on how insurance covers your medicines.) Formularies group medicines into tiers by required levels of cost sharing (generic, preferred brand, etc.). While many formularies use four tiers, an increasing number of plans are using five or more tiers or in some cases fewer than four tiers.
 So why does the number of tiers matter? Unfortunately, when health insurance exchange plans in most states report their cost sharing information, the form they use only allows plans to submit data on four-tiered formularies. That means that if a formulary has more than four tiers, the insurance company excludes information on one of those tiers from their submission. For consumers, this may mean they will see inaccurate, incomplete and potentially misleading information when shopping for coverage. When trying to compare cost sharing for prescription medicines on different plans, incomplete data is a big concern.
So why does the number of tiers matter? Unfortunately, when health insurance exchange plans in most states report their cost sharing information, the form they use only allows plans to submit data on four-tiered formularies. That means that if a formulary has more than four tiers, the insurance company excludes information on one of those tiers from their submission. For consumers, this may mean they will see inaccurate, incomplete and potentially misleading information when shopping for coverage. When trying to compare cost sharing for prescription medicines on different plans, incomplete data is a big concern.
Just how many formularies are affected by this data incompatibility issue? A recent analysis by Avalere Health of 2015 health insurance exchange plans shows that about 35 percent silver plans do not use four-tier formularies. That means one in three plans may be submitting incorrectly reported information due to the data collection tool the government created.
While having plans submit data is meant to increase transparency for consumers and make it easier to compare cost sharing across plans, it is actually misleading many of them about how what their out-of-pocket costs will be. Given one-third of plans use non-four tier formularies, when choosing a health plan, it is important that consumers review plan documents in addition to the information available from the government in order to get accurate cost-sharing requirements for their drugs. If the government is serious about giving consumers the information they need to select the right health plans, they should fix their forms so that insurers can easily provide cost sharing information on all formulary tiers.