5 Things to consider when choosing your health coverage
How much will you have to pay out of pocket before coverage kicks in? Know the questions to ask.

5 Things to consider when choosing your health coverage.
How much will you have to pay out of pocket before coverage kicks in? Know the questions to ask.

5 Things to consider when choosing your health coverage.
 Choosing a health insurance plan can feel like an overwhelming task and making sure you understand your coverage and out-of-pocket costs is important to ensure you can access the services and treatments you need. Here are five things to keep in mind when choosing health coverage for you and your family. For more information on plan components, see the Summary of Benefits and Coverage (available from an insurance company), call the insurer directly or visit the insurer’s website.
Choosing a health insurance plan can feel like an overwhelming task and making sure you understand your coverage and out-of-pocket costs is important to ensure you can access the services and treatments you need. Here are five things to keep in mind when choosing health coverage for you and your family. For more information on plan components, see the Summary of Benefits and Coverage (available from an insurance company), call the insurer directly or visit the insurer’s website.
It’s important to remember that in-network services and medicines are covered under a plan, while out-of-network services and medicines require additional out-of-pocket costs or are not covered at all. Importantly, all out-of-pocket costs for out-of-network services do not count towards a plan’s out-of-pocket maximum. Check to see if your preferred primary care or specialist provider and the pharmacy near your home are included in the plan’s network.
Premiums are the amount you pay an insurance company for coverage, whether or not you use medical and pharmacy services. Keep in mind that these are not the only costs associated with coverage. Premiums are usually paid monthly and if you stop making payments you are at risk of losing your coverage.
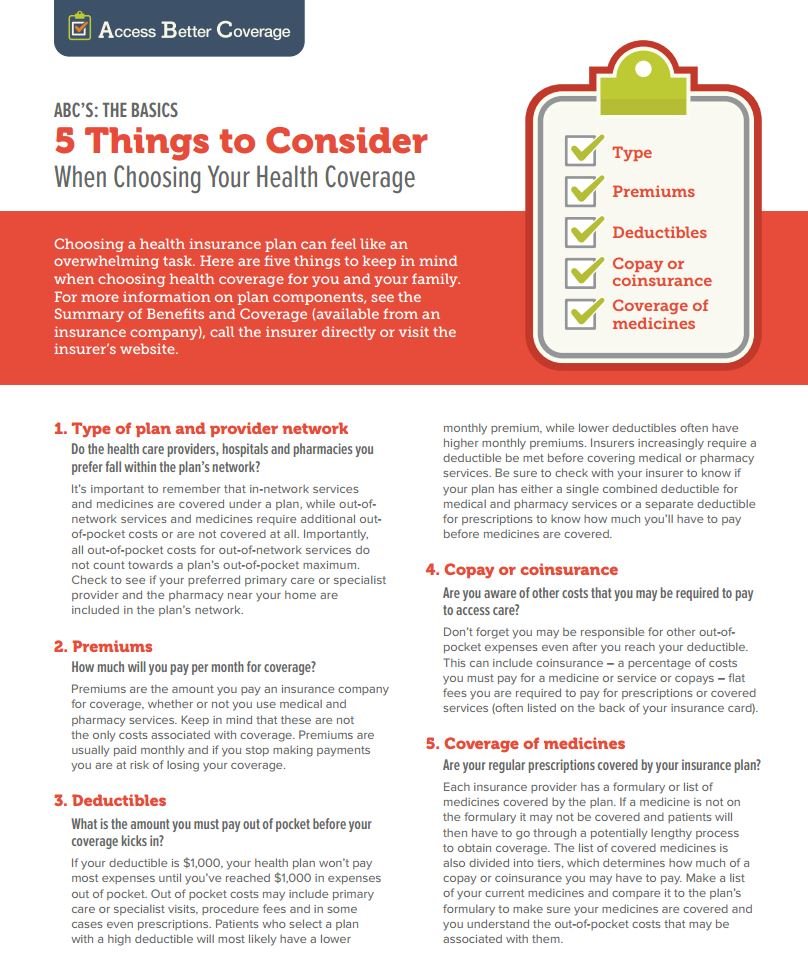 If your deductible is $1,000, your health plan won’t pay most expenses until you’ve reached $1,000 in expenses out of pocket. Out of pocket costs may include primary care or specialist visits, procedure fees and in some cases even prescriptions. Patients who select a plan with a high deductible will most likely have a lower monthly premium, while lower deductibles often have higher monthly premiums. Insurers increasingly require a deductible be met before covering medical or pharmacy services. Be sure to check with your insurer to know if your plan has either a single combined deductible for medical and pharmacy services or a separate deductible for prescriptions to know how much you’ll have to pay before medicines are covered. (Learn more about deductibles in our Glossary.)
If your deductible is $1,000, your health plan won’t pay most expenses until you’ve reached $1,000 in expenses out of pocket. Out of pocket costs may include primary care or specialist visits, procedure fees and in some cases even prescriptions. Patients who select a plan with a high deductible will most likely have a lower monthly premium, while lower deductibles often have higher monthly premiums. Insurers increasingly require a deductible be met before covering medical or pharmacy services. Be sure to check with your insurer to know if your plan has either a single combined deductible for medical and pharmacy services or a separate deductible for prescriptions to know how much you’ll have to pay before medicines are covered. (Learn more about deductibles in our Glossary.)
Don’t forget you may be responsible for other out-of-pocket expenses even after you reach your deductible. This can include coinsurance – a percentage of costs you must pay for a medicine or service or copays – flat fees you are required to pay for prescriptions or covered services (often listed on the back of your insurance card).
Each insurance provider has a formulary or list of medicines covered by the plan. If a medicine is not on the formulary it may not be covered and patients will then have to go through a potentially lengthy process to obtain coverage. The list of covered medicines is also divided into tiers, which determines how much of a copay or coinsurance you may have to pay. Make a list of your current medicines and compare it to the plan’s formulary to make sure your medicines are covered and you understand the out-of-pocket costs that may be associated with them.
Print our PDF of tips to keep handy during your enrollment period and follow @ABCsofCoverage on Twitter for more.