Ensuring that patients have access to the medicines they need is at the heart of what biopharmaceutical research companies do every day. The Affordable Care Act put in place a new way for Americans to access health insurance coverage and even provides assistance in the form of tax credits and cost-sharing reductions for those who need it most.
But while such assistance is meant to help patients get the medicines they need, which is especially critical for those managing chronic conditions like diabetes, arthritis, and heart disease, new research out today shows that many patients are not reaping this important benefit.
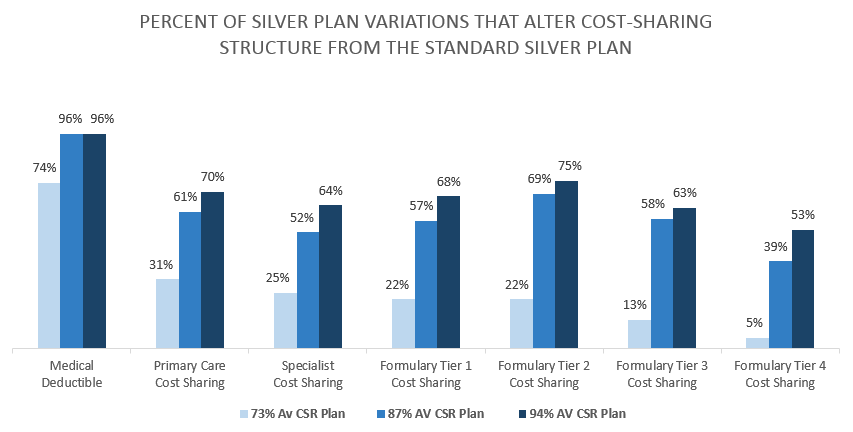
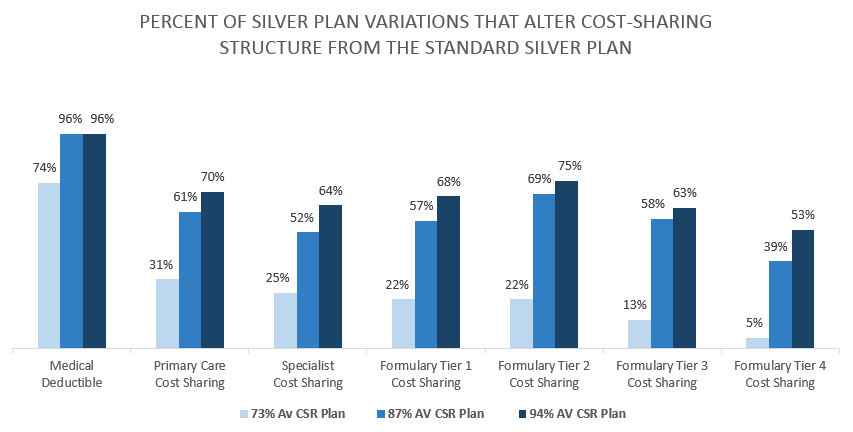
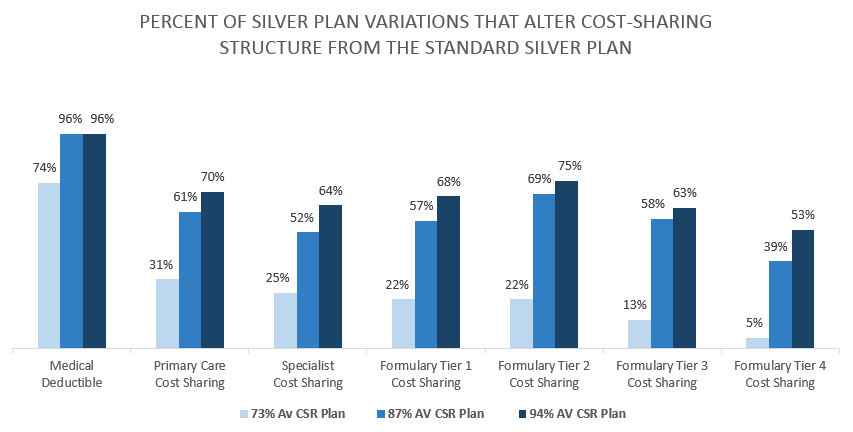 New analysis from Avalere Health looked at the types of assistance available to reduce out-of-pocket costs for consumers with health exchange coverage and found that cost-sharing reductions were not treated the same way across health insurance exchange plans. Troublingly, the research finds that in many plans, cost-sharing reductions aren’t used to lower cost-sharing for treatments or services, such as prescription medicines and physician visits. In fact, there is a wide range in how different insurance plans pass along these reductions to patients.
New analysis from Avalere Health looked at the types of assistance available to reduce out-of-pocket costs for consumers with health exchange coverage and found that cost-sharing reductions were not treated the same way across health insurance exchange plans. Troublingly, the research finds that in many plans, cost-sharing reductions aren’t used to lower cost-sharing for treatments or services, such as prescription medicines and physician visits. In fact, there is a wide range in how different insurance plans pass along these reductions to patients.
The Department of Health and Human Services has provided few constraints on how plans choose to pass cost-sharing reductions along to patients. These reductions are commonly applied to reduce deductibles or out-of-pocket caps, while most provide little to no assistance with copays or coinsurance required for medicines, especially those on the highest tier. For example, only slightly more than half of plans for the lowest-income exchange enrollees (those with incomes between about $11,700 and $17,500 for an individual) lower cost sharing for medicines on the highest tier. In 10 percent of plans, these individuals will be forced to pay coinsurance of more than 40 percent for medicines on the highest tier. These medicines often include those used to treat cancer, HIV, and multiple sclerosis, along with other chronic conditions.
This means patients who need treatments that have been placed on the top insurance tiers may face very high out-of-pocket costs for their medicines despite having coverage and cost-sharing reductions. Avalere points out that these individuals “may face barriers accessing brand-name drugs due to high cost-sharing requirements, which are particularly prevalent on higher formulary tiers.”
Cost-sharing reductions are meant to help low-income patients better afford health coverage through the exchanges, but instead, plans are allowed to continue to require high out-of-pocket costs for medicines, which can ultimately limit patient access to needed treatments. As the health care system continues to look for ways to contain costs, barriers to medicines must be removed. Research proves that better patient adherence to medicines helps avoid other, more costly care, such as hospitalizations and surgeries.
View the full report here. (Note: The analysis was funded by PhRMA. Avalere maintained editorial control over the content of the analysis and release.


 New analysis from
New analysis from 