Last week, we looked at access to medicines in health insurance exchanges for HIV/AIDS, oncology, cystic fibrosis, mental health and multiple sclerosis. The analysis by Avalere Health presents data on access to medications for chronic conditions in exchange plans.
Last week, we looked at access to medicines in health insurance exchanges for HIV/AIDS, oncology, cystic fibrosis, mental health and multiple sclerosis. The analysis by Avalere Health presents data on access to medications for chronic conditions in exchange plans.
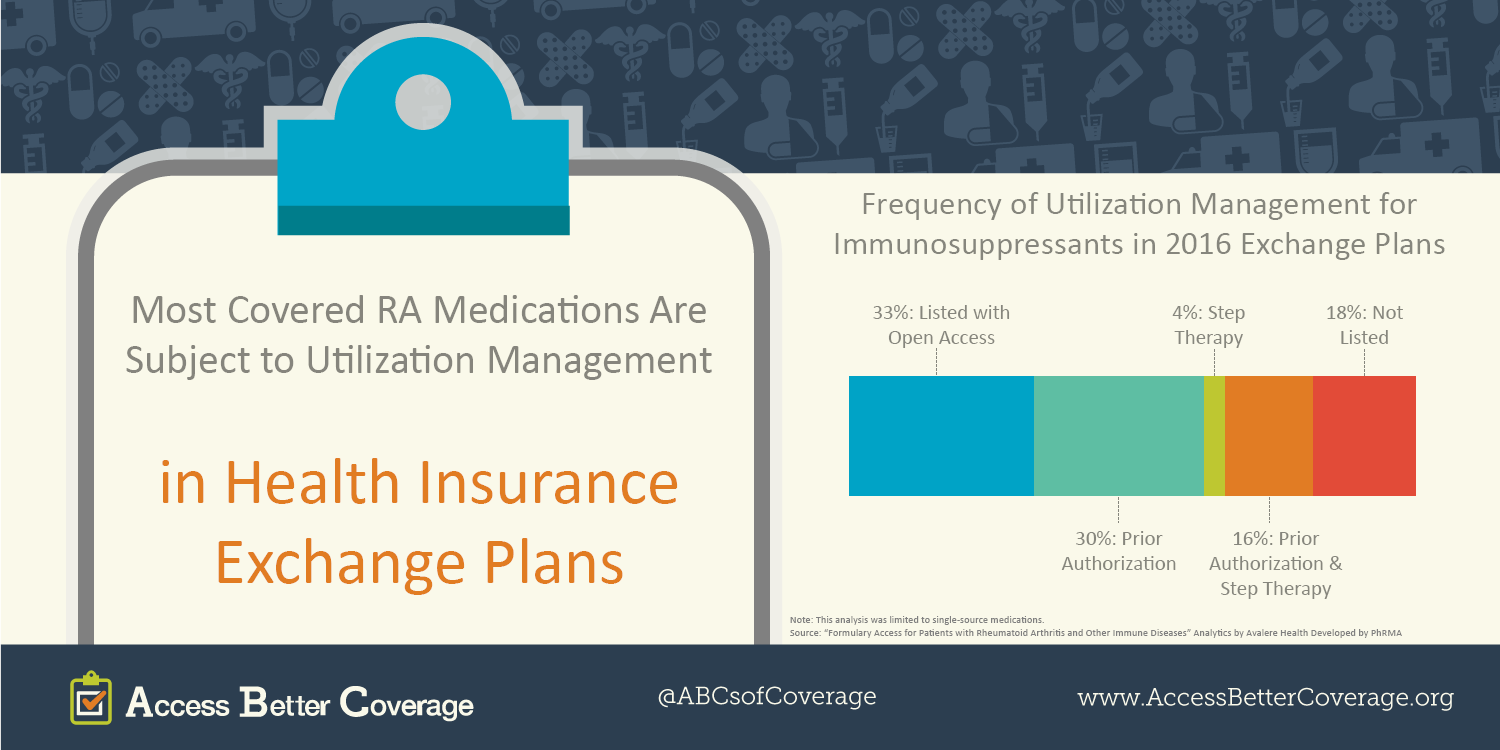
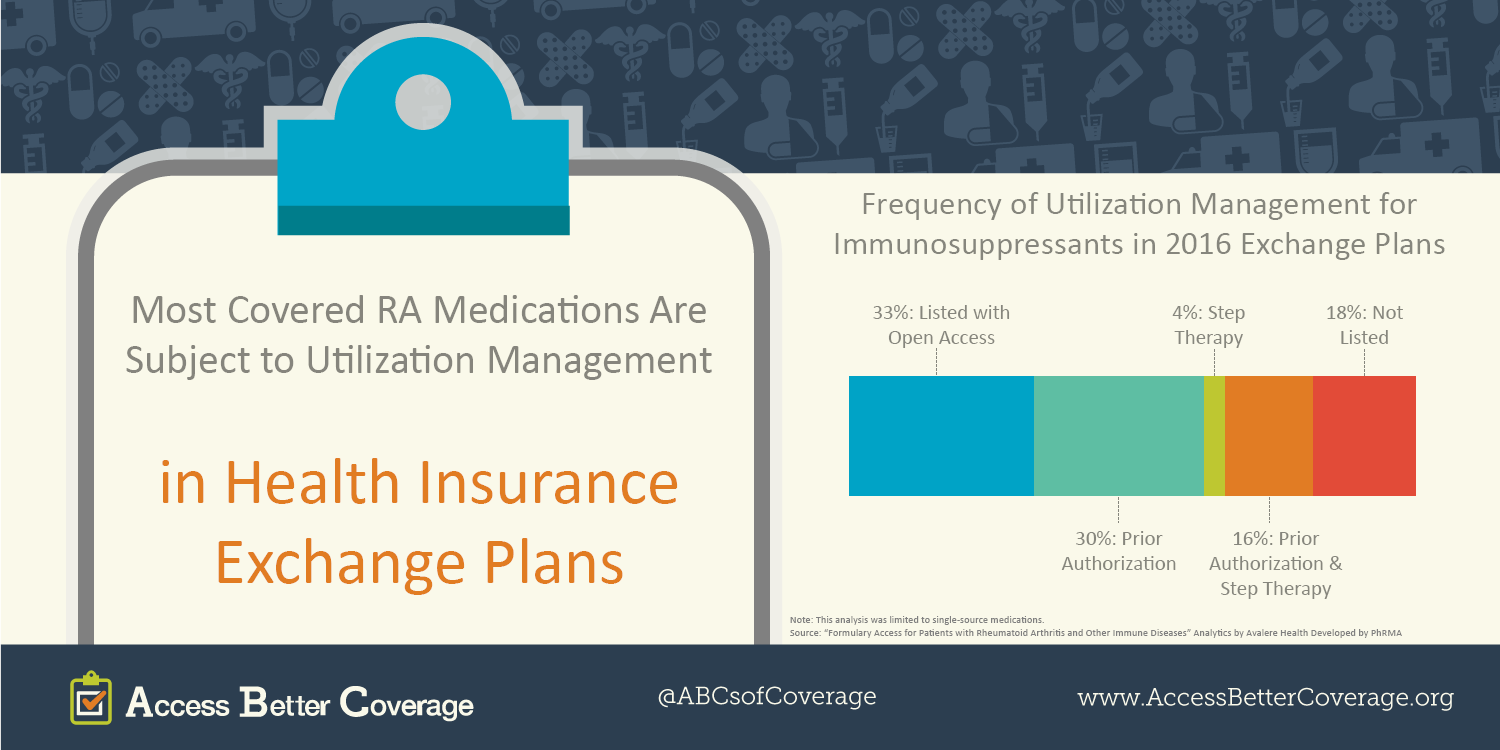
Today, we’re looking at five more conditions and how insurance benefit design – and practices like utilization management – can be a hurdle to patients with chronic conditions accessing the medicines they need. Utilization management can mean prior authorization, where your health care professional has to get approval from your insurance company, or step therapy, where you might have to fail first on older or less personalized medicines before the medicine you are prescribed is covered.
- Rheumatoid arthritis (RA) and other autoimmune diseases: In the majority of cases, when an RA drug is covered by an exchange plan, it is subject to utilization management.
- Hepatitis: While coverage of hepatitis medicines improved, so did the use of utilization management for these medicines, up from 47 percent of the time in 2015 to 57 percent of the time in 2016.
- Hyperlipidemia (high cholesterol): Utilization management is used for these medicines more than one third of the time in health insurance exchange plans.
- Diabetes: Innovative diabetes medicines are more often placed on a non-preferred tier in health insurance exchange plans, and there is greater use of utilization management in exchange plans compared to employer plans.
- Asthma and COPD: Utilization management for these medicines is low compared to other conditions, but remains higher than employer coverage.
Health insurance exchange coverage of medicines also varies greatly by state. Check out the map and state-specific fact sheets here.



 Last week, we looked at access to medicines in health insurance exchanges for
Last week, we looked at access to medicines in health insurance exchanges for