Despite warnings from the Centers for Medicare & Medicaid Services (CMS) that requiring high cost sharing for all or most medications to treat a condition may be discriminatory, new data from Avalere show some health plans are continuing to engage in this practice. While the share of plans with this type of formulary design has generally decreased, we are still seeing some plans placing all medicines for some conditions on the specialty tier or on a tier with high coinsurance. Surprisingly, this is sometimes occurring even in drug classes where there are generics available. Placing all medicines on the highest cost-sharing tier—a practice known as adverse tiering—can lead to thousands of dollars in additional out-of-pocket costs even for patients taking generic medicines.
Despite warnings from the Centers for Medicare & Medicaid Services (CMS) that requiring high cost sharing for all or most medications to treat a condition may be discriminatory, new data from Avalere show some health plans are continuing to engage in this practice. While the share of plans with this type of formulary design has generally decreased, we are still seeing some plans placing all medicines for some conditions on the specialty tier or on a tier with high coinsurance. Surprisingly, this is sometimes occurring even in drug classes where there are generics available. Placing all medicines on the highest cost-sharing tier—a practice known as adverse tiering—can lead to thousands of dollars in additional out-of-pocket costs even for patients taking generic medicines.
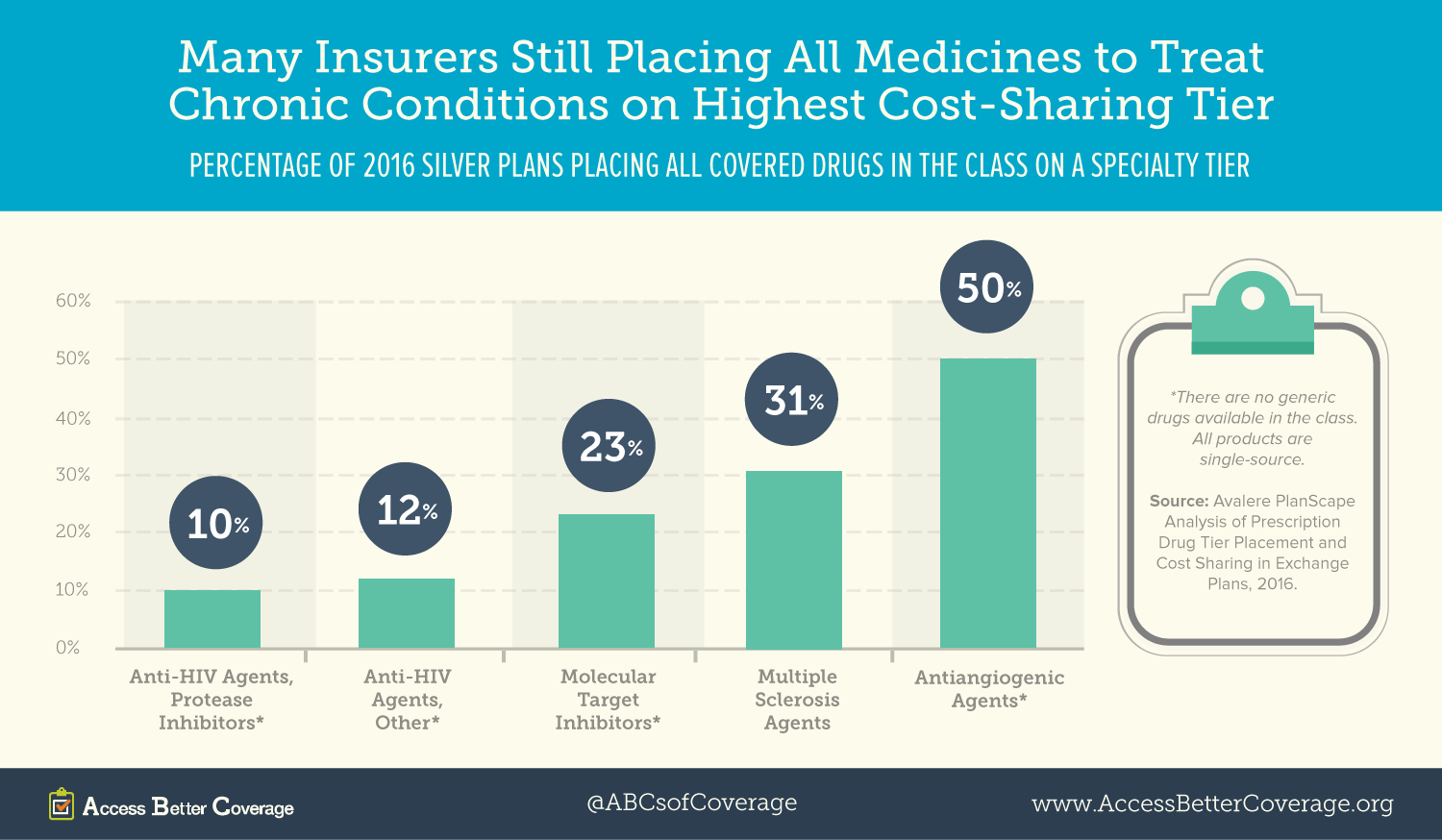
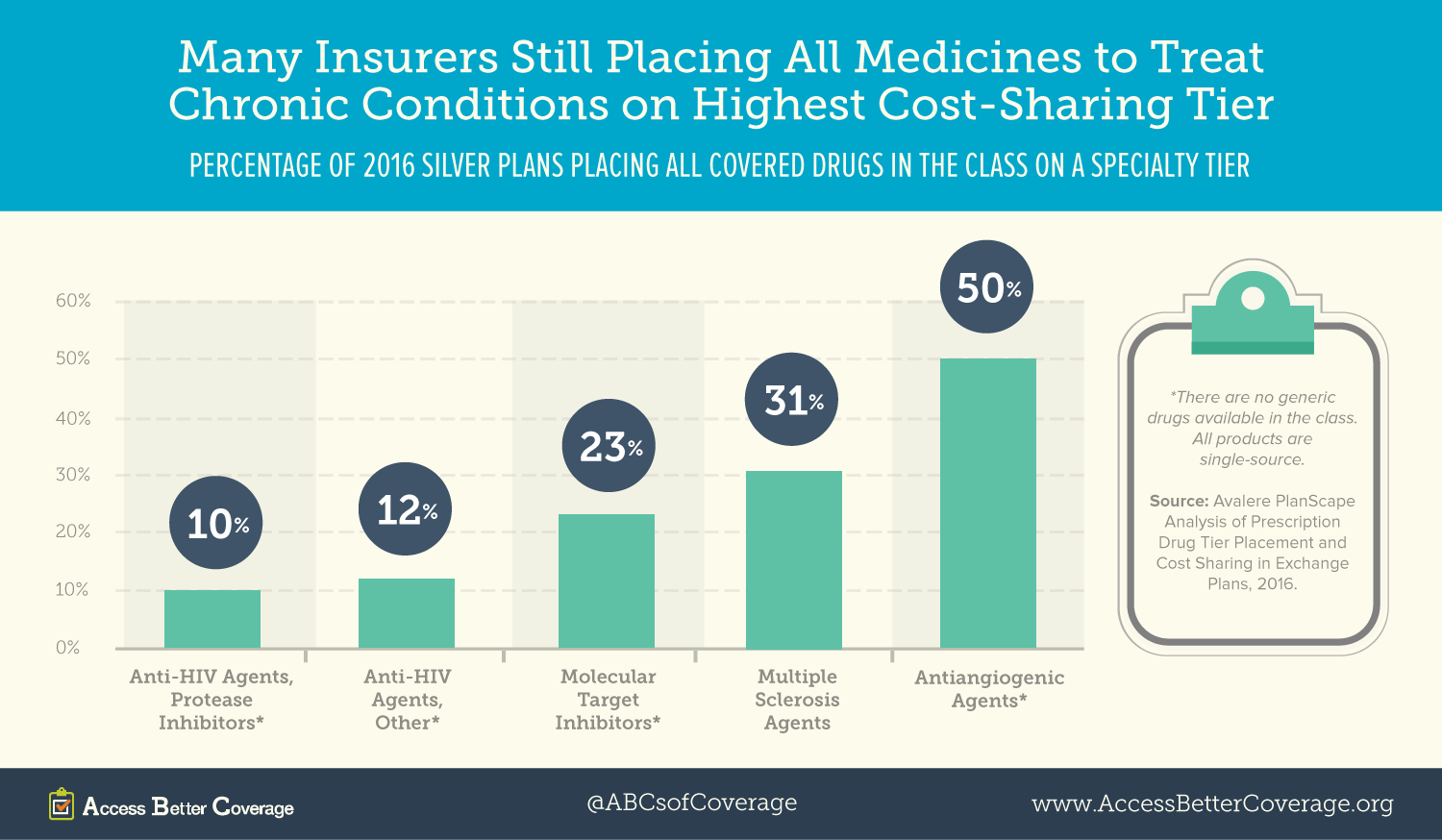
In 2016, half (50 percent) of health plans put all cancer medicines in the antiangiogenic agents class on the specialty tier (see figure 1) and almost one-third (31 percent) of plans engage in the same practice for multiple sclerosis medicines. Further, about 1 in 10 health plans are placing all HIV medicines in certain classes on the specialty tier. Avalere also found some silver plans require cost sharing of more than 40 percent for all medicines in certain classes, meaning, despite having coverage, a patient is on the hook for 40 percent of the costs out of pocket or they cannot get their medicine. Silver plans are the most popular health plans in the exchanges and are designed to cover an average of about 70 percent of total allowable health care costs.
The adverse tiering still occurring in the marketplace suggests insurance issuers may be using their formularies to discourage patients with certain conditions from enrolling in their health plans. The Affordable Care Act is supposed to protect against this type of discrimination, but states may not have the resources or technical expertise to identify potentially discriminatory formularies. CMS is now considering changes to the risk adjustment mechanism that is supposed to compensate plans for enrolling people at higher risk of needing costly medical care. Those improvements could help reduce the incentives for adverse tiering and allow plans to concentrate on effectively managing chronic conditions. Learn more about this and other policy solutions to engage and empower consumers here.



 Despite warnings from the
Despite warnings from the