Blog


Accumulator adjustment programs lead to surprise out-of-pocket costs and nonadherence, analysis finds
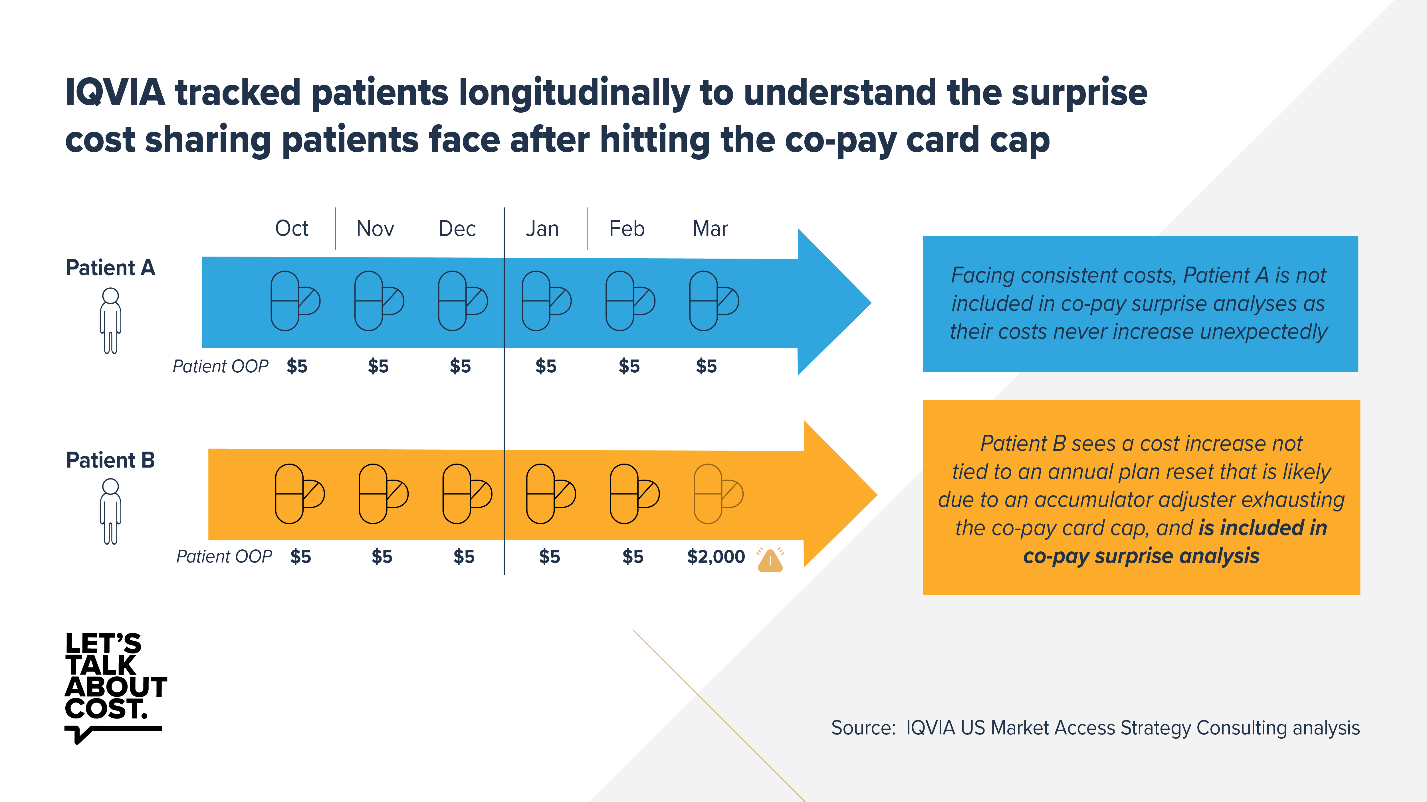
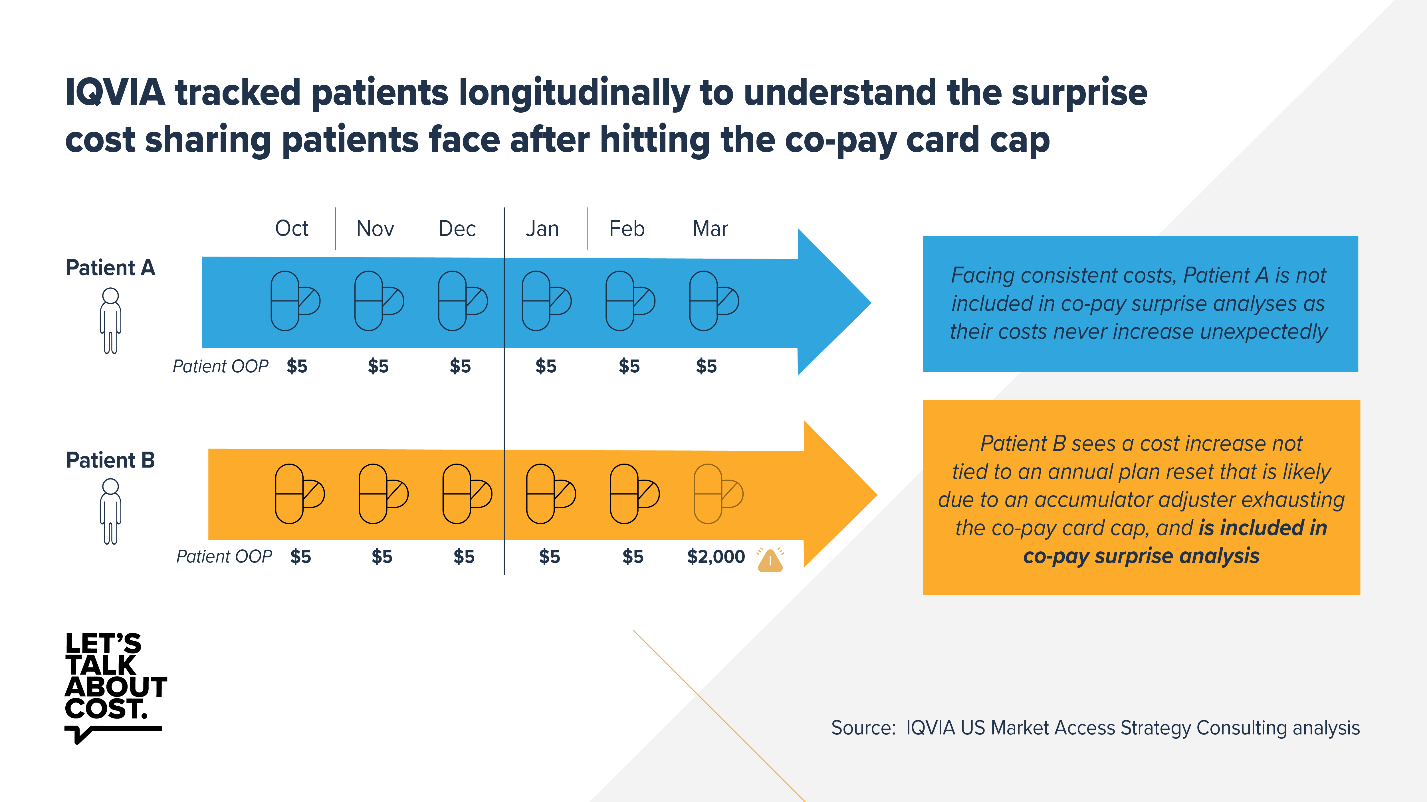
A new analysis by IQVIA looked at three cost-sharing assistance programs and found that from 2018 to 2020, 25% to 36% of patients discontinued treatment when they faced an unexpectedly high out-of-pocket cost of $1,500 or more in the middle of the plan year. These unexpected costs were caused by accumulator adjustment programs operated by pharmacy benefit managers and health plans.
Accumulator adjustment programs exclude cost-sharing assistance from patients’ deductibles and out-of-pocket maximums. When their cost-sharing assistance runs out, patients may face surprise out-of-pocket costs, commonly known as a “copay surprise,” where they find out that their insurer doesn’t count the cost-sharing assistance toward their deductible or other out-of-pocket maximums. This can leave patients with unexpected out-of-pocket costs that they may not be able to afford, prompting many to abandon treatment, which in turn may lead to negative health outcomes and drive up future health costs.
According to a 2020 Managed Markets Insight & Technology survey of health plans, payers covering 52% of commercial market enrollees were responsible for health plans that implemented accumulator adjustment programs on at least some medicines, meaning that millions of Americans are at risk for surprise out-of-pocket costs at the pharmacy counter. In the past year alone, middlemen have tripled the use of these programs.
Evidence suggests that nonadherence caused by accumulator adjustment programs can negatively impact patients’ physical and financial health. A previous analysis found that most patients who abandon their prescriptions do not fill any other prescription within three months, suggesting that they are not using a lower cost medicine but are instead failing to start treatment as prescribed by their physician. Considering that 44% of Americans would have trouble paying an unexpected $400 emergency expense, the implications of accumulator adjustment programs on medication adherence are likely significant. Insurance should not be a roadblock for patients to get the medicines they need.
We need to enact policies requiring plans to count cost-sharing assistance toward out-of-pocket limits rather than excluding it from these calculations. Cost-sharing assistance is vital for patients facing large deductibles or coinsurance set by health plans – sometimes saving patients hundreds to thousands of dollars annually. In fact, the National Hemophilia Foundation found that 86% of all registered voters who were surveyed believe the government should require cost-sharing assistance to be applied to a patient’s out-of-pocket costs. In two back-to-back regulatory actions in recent months, the Administration has taken steps to make it harder for biopharmaceutical companies to offer assistance to commercially insured patients. Rather than rushing to advance policies that could ultimately increase patients’ financial burdens, the Administration should fully consider the negative impacts these changes could have on patients and stop their assault on cost-sharing assistance.
Learn more at letstalkaboutcost.org.
- Adherence,
- Drug Cost,
- Patient Assistance Programs,
- Out-of-Pocket Costs,
- Lets Talk About Cost

 Gabby Migliara
Gabby Migliara