We are committed to engaging a wide range of audiences and having a dialogue on opportunities to create a better health care system. We believe health literacy can not only help patients make appropriate decisions about their own health but also help enable constructive conversations on how we can support a regulatory and policy environment that helps patients access life-saving medications. In this ongoing series, we are choosing to spotlight terms fundamental to the biopharmaceutical ecosystem and illustrate their significance in promoting innovation and timely patient access to medicines. This week, we are taking a look at the critical role biomarkers and surrogate endpoints play in enhancing the drug development process.
What is a biomarker?
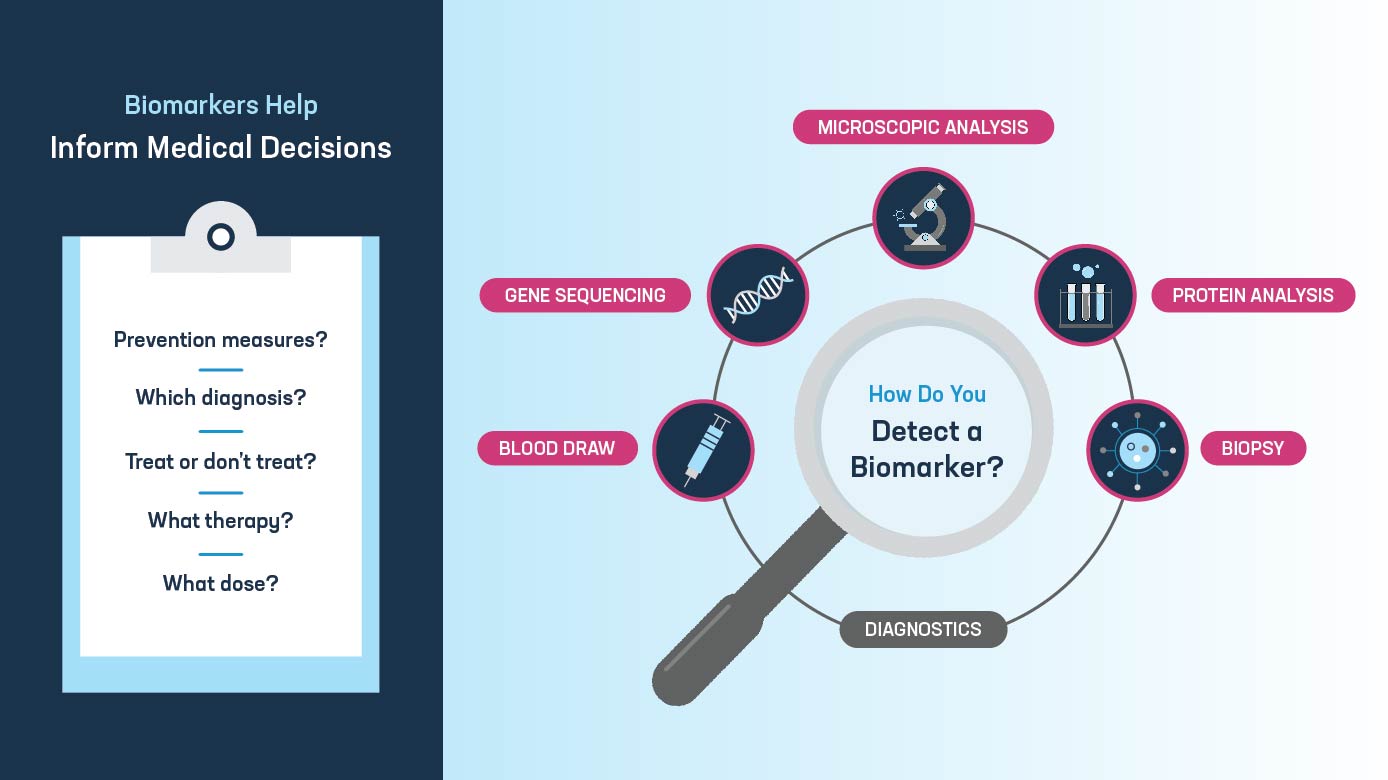
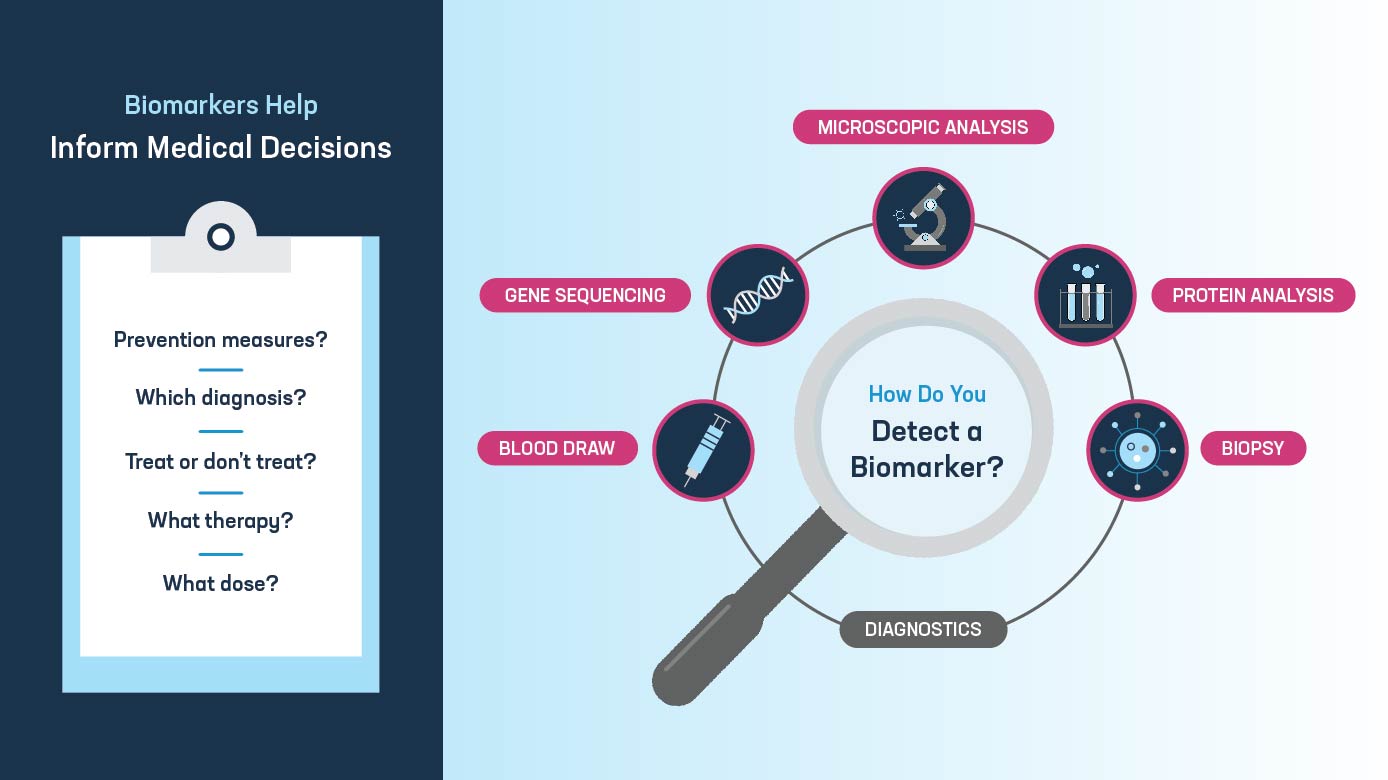
A biomarker (short for biological marker) is a measure or physical sign used to evaluate how the body is functioning. Biomarkers have multiple applications in health care, including diagnosing diseases, understanding how a disease progresses and measuring how a body is responding to a treatment. An example of a biomarker in action is the use of blood sugar levels to help identify and monitor patients with diabetes and indicate how their body may react to a change in diet or treatment.
Biomarkers are also key tools in the development of therapeutics and can enable patient selection and stratification in clinical trials, allowing science-informed trial design through target selection. Furthermore, biomarkers have applications in developing companion diagnostics to help identify patients who are most likely to benefit from a given medicine, resulting in personalized medicine successes.
What is a surrogate endpoint?
A surrogate endpoint is a measure — which can include a biomarker or other physical sign — that is used as a substitute for a direct measure of how a patient feels, functions or survives, and is expected to predict that direct clinical response.
Before the FDA approves a new medicine, a sponsor must demonstrate that the treatment is safe and effective. This is principally demonstrated by a clinical trial meeting specific measures called clinical endpoints. A surrogate endpoint may be used as a substitute for a clinical endpoint in some clinical trials. This can be helpful for highly complex or slowly progressing diseases in which clinical endpoints are not always available.
Surrogate endpoints are sometimes used to support approvals under the FDA’s accelerated approval pathway, which enables expedited access to medicines that address an unmet medical need for serious and life-threatening diseases and conditions while preserving the FDA’s high standards for safety and effectiveness. As such, the use of surrogate endpoints can help connect patients with earlier access to lifesaving therapies.
How can biomarkers and surrogate endpoints improve the drug development process?
Continuing advances in science and genomics are driving an increased understanding of human physiology and how diseases affect the body; these advances are helping researchers identify new biomarkers. As more biomarkers are identified, they have the potential to greatly enhance the drug development process by providing researchers with new ways to measure disease activity, reduce the amount of time required to show a medicine is safe or effective and enable the development of more personalized treatments — particularly where multiple biomarkers can inform the use of targeted drug combinations. Biomarkers can also allow researchers to better understand how effective a treatment is against a disease with endpoints that are difficult to define, providing clinicians with additional informative measurements in the early diagnosis of a disease and identify differences in responses between individuals or subpopulations.
Furthermore, the development of personalized medicines that are more tailored to the individual patient using biomarkers helps drive efficiencies and improvements in patient care. That is because biomarkers can help identify those most likely to benefit from a specific treatment. For example, biomarkers are often used in cancer treatments to identify patients with tumors expressing certain genetic characteristics that indicate those patients are likely to respond to a targeted cancer therapy.
What is the future of surrogate endpoints and biomarkers?
To harness the full potential of biomarkers, researchers need assurance from the FDA that a specific biomarker is an acceptable measure as a surrogate endpoint. The FDA’s Prescription Drug User Fee Act (PDUFA VII) Commitment Letter includes dedicated resources for the FDA to provide early consultation on the use and qualification of a biomarker as a new surrogate endpoint to support accelerated or traditional approval.
Looking ahead, we urge policymakers to move on swiftly reauthorizing the PDUFA program, as well as the Biosimilar User Fee Act (BsUFA III), before the current user fee reauthorizations expire on September 30. Acceptance of biomarkers and the use of surrogate endpoints can open new avenues for treating complex diseases, including those in which there is a significant unmet medical need. Delivering on this promise is dependent on a modern regulatory framework, supported by PDUFA and BsUFA, that provides assurance and predictability for biopharmaceutical industry researchers.