Last year, PhRMA was joined by patient groups to highlight an analysis that found a majority of plans in health insurance exchanges required relatively high cost sharing for all medicines in at least one class. The cost burden leaves many patients with no other option, forcing them to make tough choices or go without needed medicines, ultimately having a negative impact on their health.
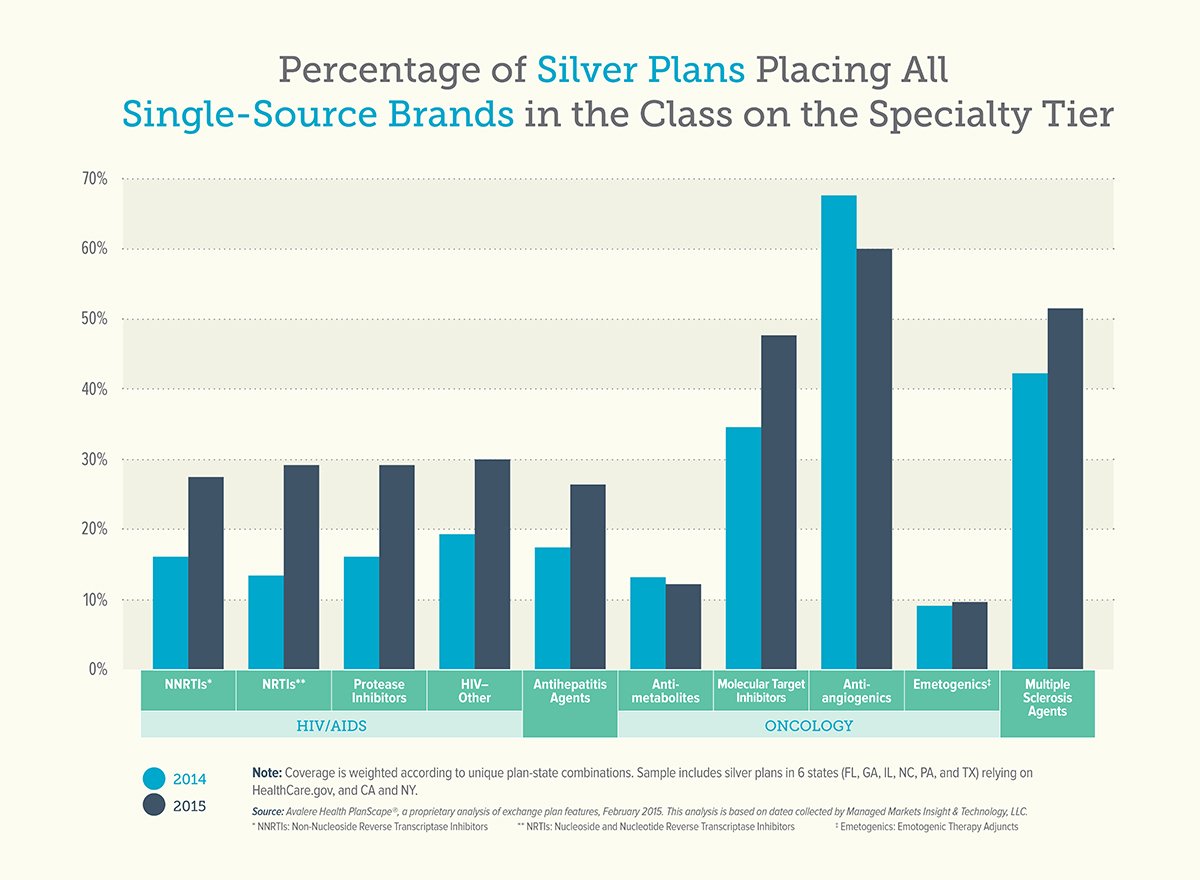
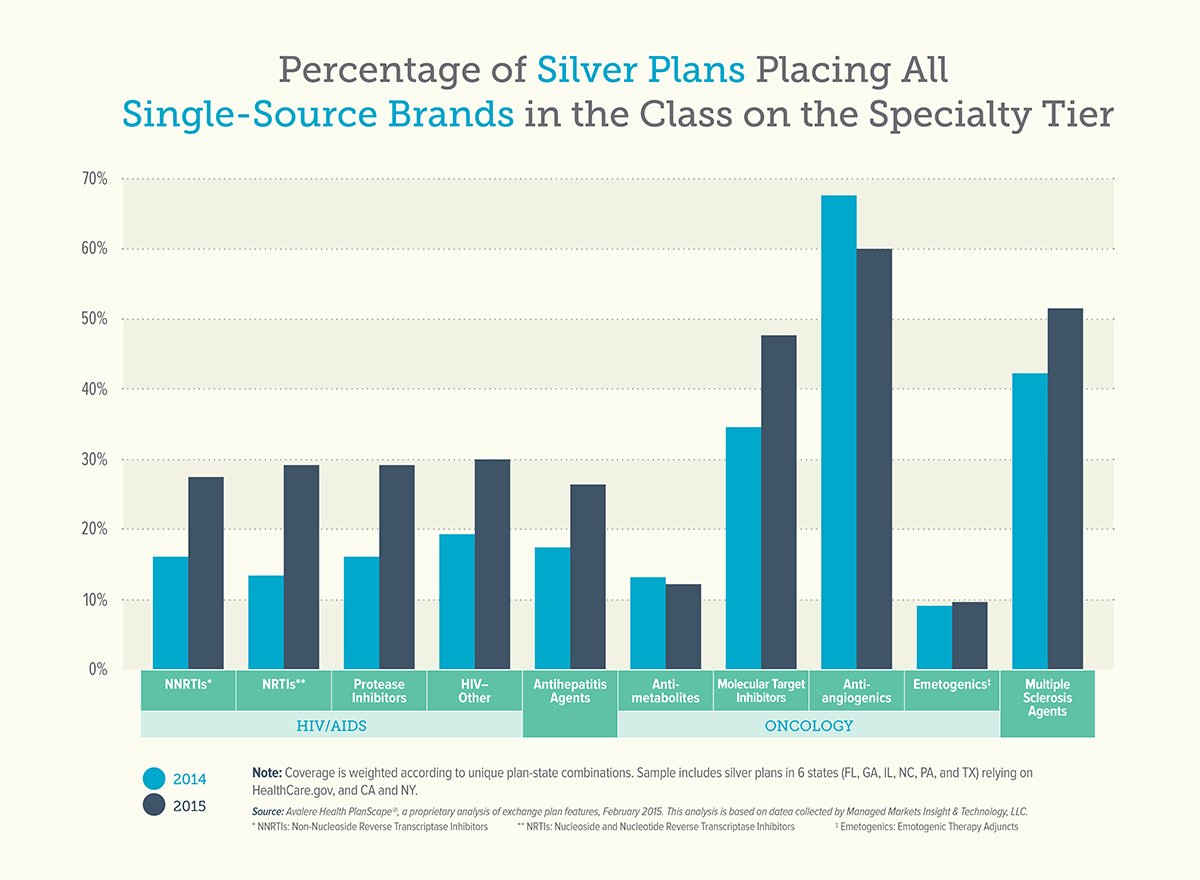
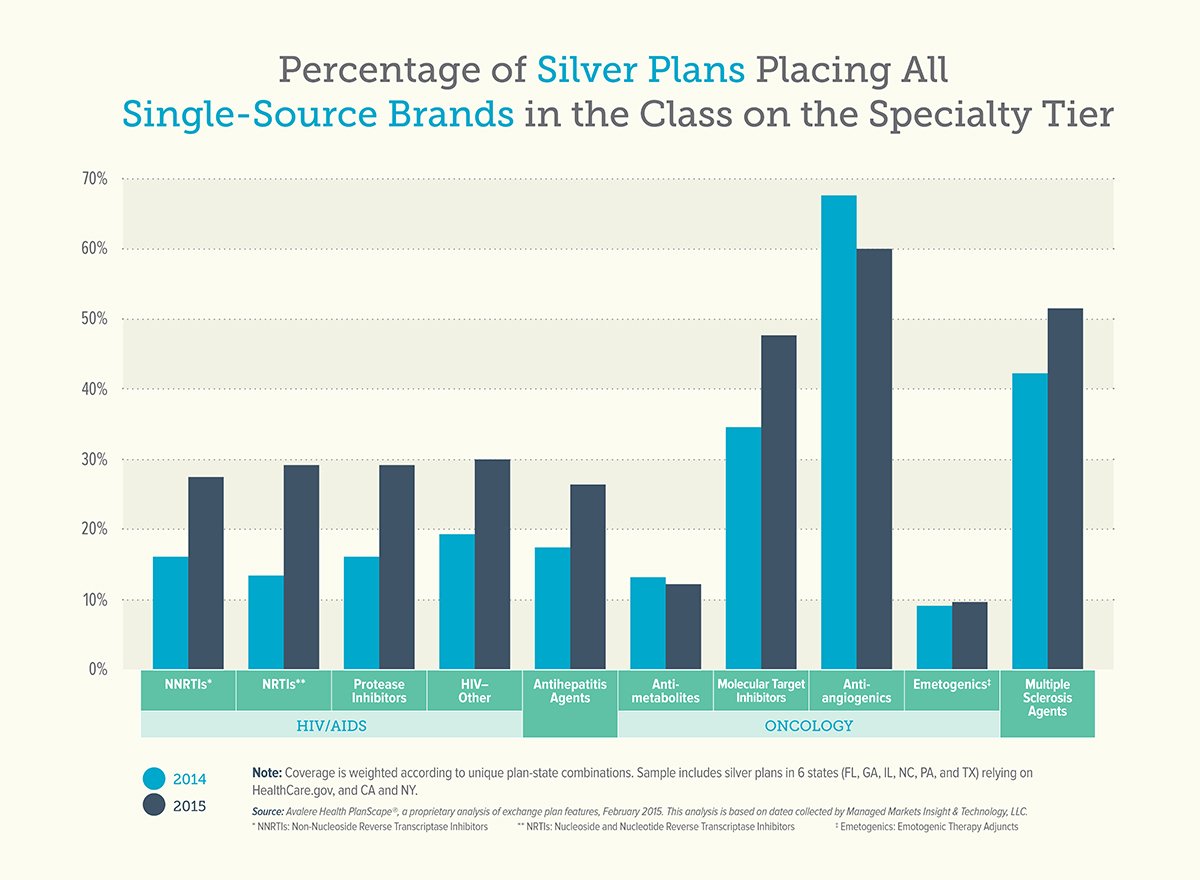
Today, Avalere Health released a new analysis of 2015 health insurance exchange plan formularies and the results are disappointing. The percentage of plans placing all medicines to treat a chronic disease on the top tier increased in 2015. For medicines to treat HIV/AIDS, the number of plans placing all treatments on the top formulary tier nearly doubled. This practice is continuing even in drug classes where generics are available.
We remain concerned about patient access to medicines in health insurance exchange plans and this new analysis highlights the increasing rate at which insurers are using discriminatory practices at the expense of patients with chronic conditions. While the administration has acknowledged that placing all or most medicines on the highest cost tiers is discriminatory, now is the time to take the next step to ban this discriminatory practice.