How do multiple sclerosis patients define value?
How do multiple sclerosis patients define value?.
How do multiple sclerosis patients define value?.

There are crucial conversations occurring in the health care system about how value is defined. To explore how multiple sclerosis (MS) patients, providers and payers view value, Real Endpoints conducted research that found significant variability in treatment preferences among MS patients, as well as a difference in how patients define value in MS therapies compared to payers and physicians.
It is widely acknowledged that patients with MS are different in terms of clinical needs, preferences and treatment goals. For MS patients, providing greater opportunity for successful management of the disease and its progression requires the availability of a broad range of therapeutic alternatives. Often, a treatment option that is effective and has few side effects in one MS patient may produce the opposite result in another due to the diverse nature of the disease. Additionally, different patients may require different treatments depending on their preferences or treatment goals – some patients may place more weight on slowing disease progression, while others may be concerned about safety and side effect profiles. Fortunately, as a result of treatment advances over the past several decades, a range of options are now available to meet the wide variety of needs of people with MS.
The variability in treatment needs and preferences among MS patients found in Real Endpoint’s research is also why population-level judgements of an MS treatment’s value, like the recent value assessment conducted by the Institute for Clinical and Economic Review (ICER), often fail to capture the true importance of these medicines to patients. ICER’s payer-centric value assessment also doesn’t capture significant differences in what patients value in MS treatments compared to what payers value in how MS patients are treated. If misused by payers and policymakers, ICER’s assessment could also impede successful management of MS by limiting patient and provider choice, which is critical to managing and slowing progression of the disease.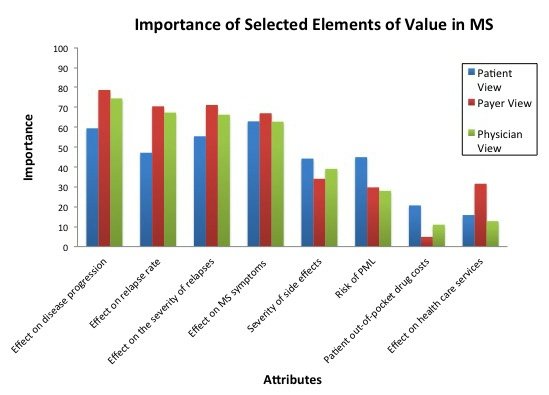
(Source: Real Endpoints, LLC, January 2017)
Key findings from Real Endpoints’ research include:
More information on Real Endpoints’ findings can be found here.