The Department of Health and Human Services recently proposed a rule that would encourage using discounts negotiated between biopharmaceutical manufacturers and Part D plans to reduce patients’ out-of-pocket costs at the pharmacy counter. This could save patients hundreds of dollars each year, especially those with chronic diseases like diabetes, rheumatoid arthritis and hepatitis C.
Today, we’re highlighting how the proposed rule could help patients like Anthony and Frank, two hypothetical Medicare Part D beneficiaries[i], by increasing cost sharing savings and improving the value of their Part D coverage.
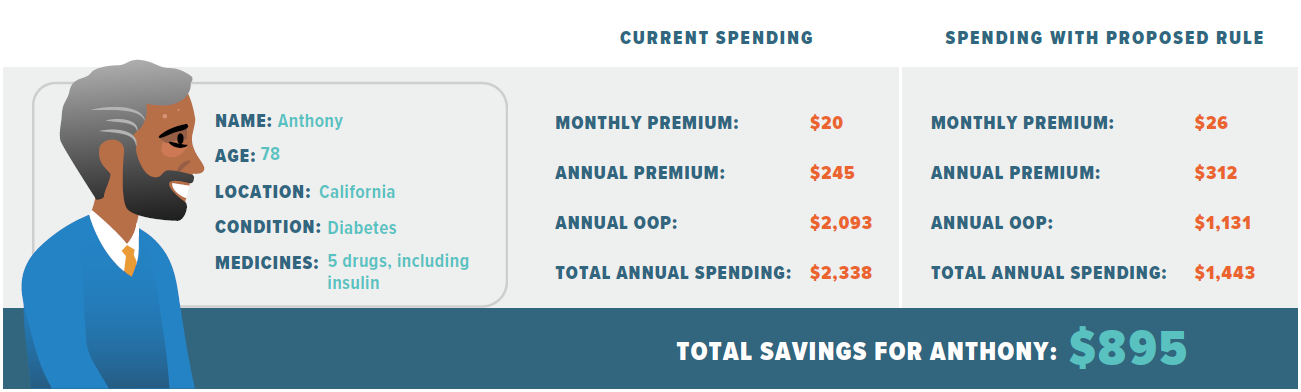
Anthony is a 78-year-old from California who has been managing diabetes for several years. He takes five medications, including insulin, and is projected to spend $2,338 on his medications and Part D premiums this year due to steep cost sharing amounts. Today, cost sharing amounts are tied to the list price of medicines, even though insurers are charged far less.
However, the rebate rule proposal would help patients like Anthony by reducing out-of-pocket costs at the pharmacy. While Anthony’s average monthly premium may increase by up to $6, the proposed rule could lower his annual out-of-pocket costs to $1,131, contributing to $895 in total savings.
Frank, a 65-year old from Texas, has hepatitis C. He takes two medications, including a brand direct-acting antiviral, to manage his condition. Like Anthony, Frank incurs high out-of-pocket costs for his medications, which are projected to total $6,800 by the end of the year. If the rebate rule is enacted, however, Frank’s out-of-pocket spending could decrease to $3,419 – almost half of what he’s paying now.

When Frank and Anthony’s cost sharing goes down, the value of their insurance goes up. Actuaries and government scorekeepers expect the proposed rule to decrease the Part D deductible and lower the amount of spending required to reach the catastrophic coverage phase. This would ultimately increase the value of Part D coverage for all seniors, even those who just take generic medicines. Moreover, when patients are better able to afford their medicines, evidence shows health outcomes improve and Medicare saves money overall.
In addition to lowering out-of-pocket costs and increasing the value of Anthony and Frank’s insurance coverage, the proposed rule would shift incentives to favor lower cost medicines and drive market competition. As policy makers continue to discuss changes to Medicare Part D, it is imperative to focus on changes that drive competition in the marketplace, lower out-of-pocket costs and improve access to the critical treatments and cures of today, as well as the future.
Visit PrescriptionForMedicare.org to learn more about how HHS proposed rebate rule is the right prescription for Medicare.
[i] NOTE: Calculations by Avalere Health reflect the 2019 parameters for non-LIS beneficiaries in actual standalone PDPs. Proposed rule adjustments assume premium increases as projected by OACT and reduce each brand drug's negotiated price by its average non-Medicaid list-to-net discount as reported by SSR Health.