Stakeholder after stakeholder has raised concerns that the Department of Health and Human Services’ proposed International Pricing Index (IPI) Model would put patient access to medicines in Medicare Part B at risk – medicines that are necessary to treat complex conditions like cancer, rheumatoid arthritis and autoimmune diseases. One of the most common concerns is that patients in the United States will experience the same access restrictions that patients face abroad if the U.S. government proceeds with copying the flawed pricing practices of foreign governments. Recently, IHS Markit released a study that shows the effect that reduced access to medicines has on patient outcomes. As a chorus of groups has stated, it is likely we will see similar harm to patient access and outcomes in the United States if the proposed IPI model moves forward.
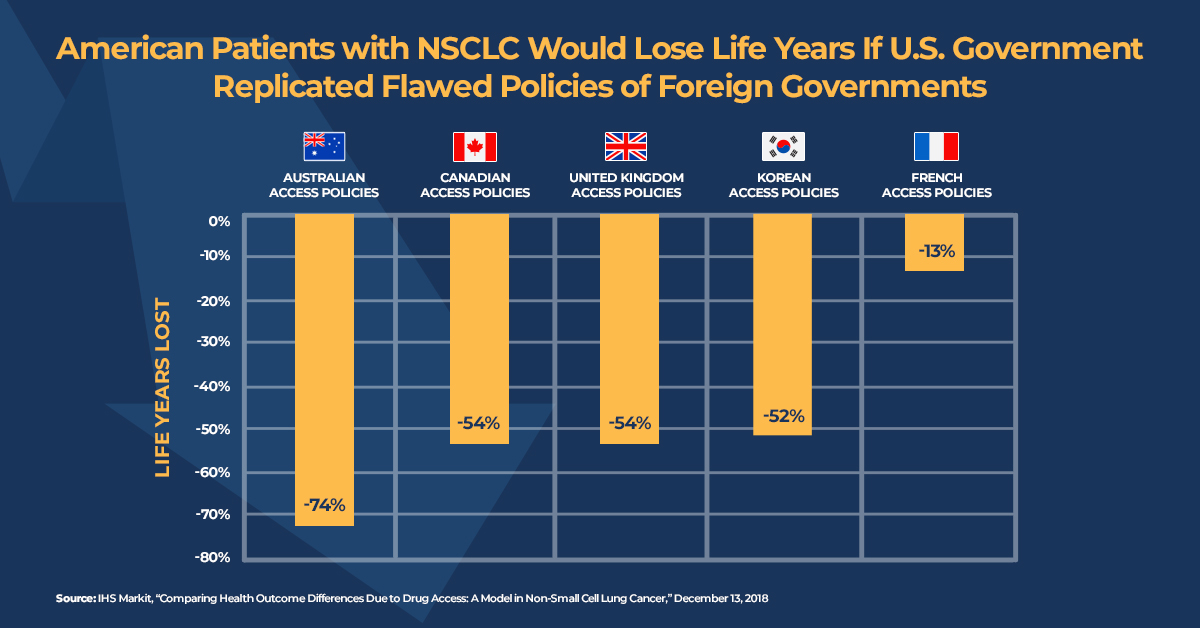
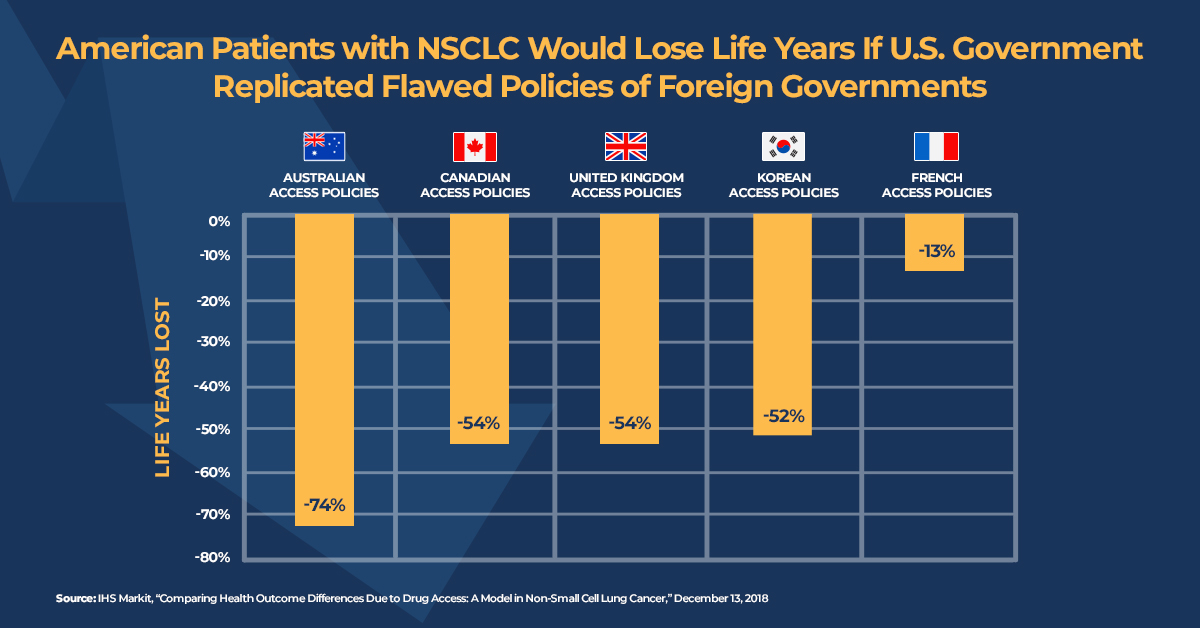
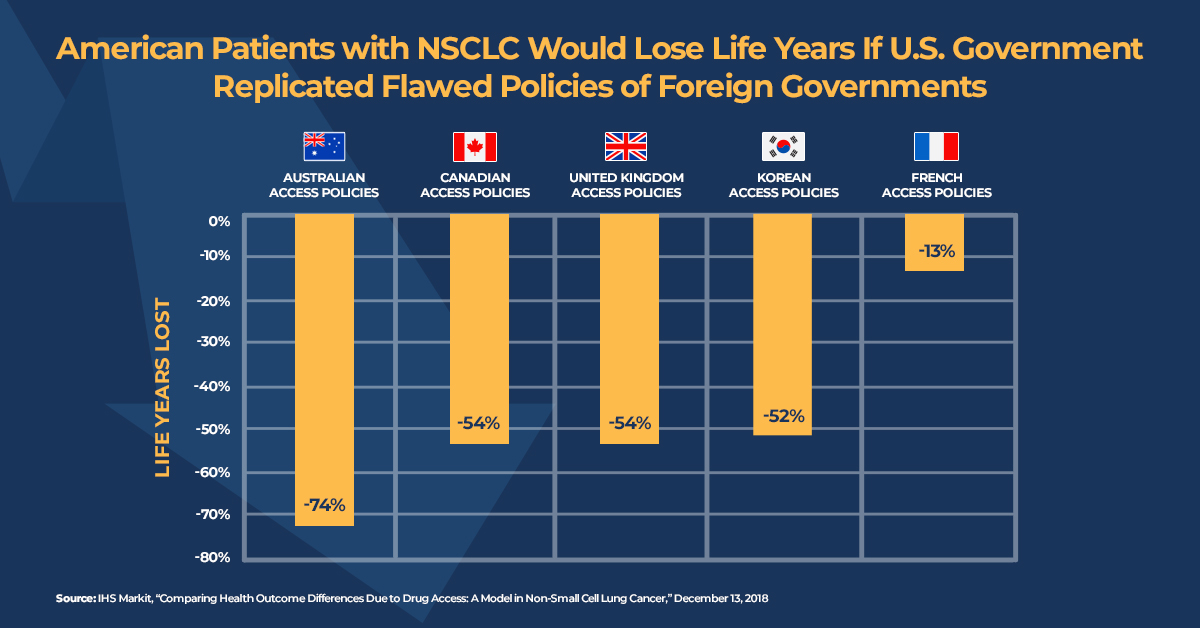
The IHS Markit analysis estimated the impact of innovative treatments for locally advanced or metastatic non-small cell lung cancer (NSCLC) in the United States from 2006 to 2017. The study then estimated treatment gains if American patients faced the access restrictions found in five foreign countries (Australia, Canada, France, South Korea and the United Kingdom) that rely on health technology assessment frameworks to decide access to medicines. The analysis shows that U.S. patients gained 201,700 life years in total due to innovative medicines being made available with little to no delay after regulatory approval.
According to IHS Markit, Americans diagnosed with locally advanced or metastatic NSCLC between 2006 and 2017 would have lost half of their survival gains if the United States adopted health technology assessment frameworks like those used by foreign governments to determine access to care – meaning half of the life years they gained from new treatments.
This is just the latest piece of evidence demonstrating the very real threat to health outcomes posed by the IPI model. The White House Council of Economic Advisers released a report in October that also concluded replicating foreign policies would be bad for American patients. Specifically, the report found increases in mortality for patients 55 and older in the United States if European-style price controls were adopted here.
In addition, the administration's suggestion that the IPI model would lower out-of-pocket costs for seniors does not tell the whole story. Avalere conducted a study and concluded most seniors will not see a reduction in out-of-pocket costs. In fact, Avalere estimates that, if the model included the 27 medicines listed in the Office of the Assistant Secretary of Planning and Evaluation report, less than 1 percent of seniors in Medicare would potentially see reduced out-of-pocket costs. This analysis takes into account that more than 87 percent of Part B beneficiaries have supplemental insurance to cover their out-of-pocket costs.
Study after study underscores that the administration should stop this harmful proposal and instead pursue reforms that strengthen market competition and the move toward value-based care, which can control costs while supporting better outcomes for patients.