According to our inaugural Patient Experience Survey (PES), insurance design can jeopardize patients’ health due to access barriers to medicines.
Here are three things you should know.
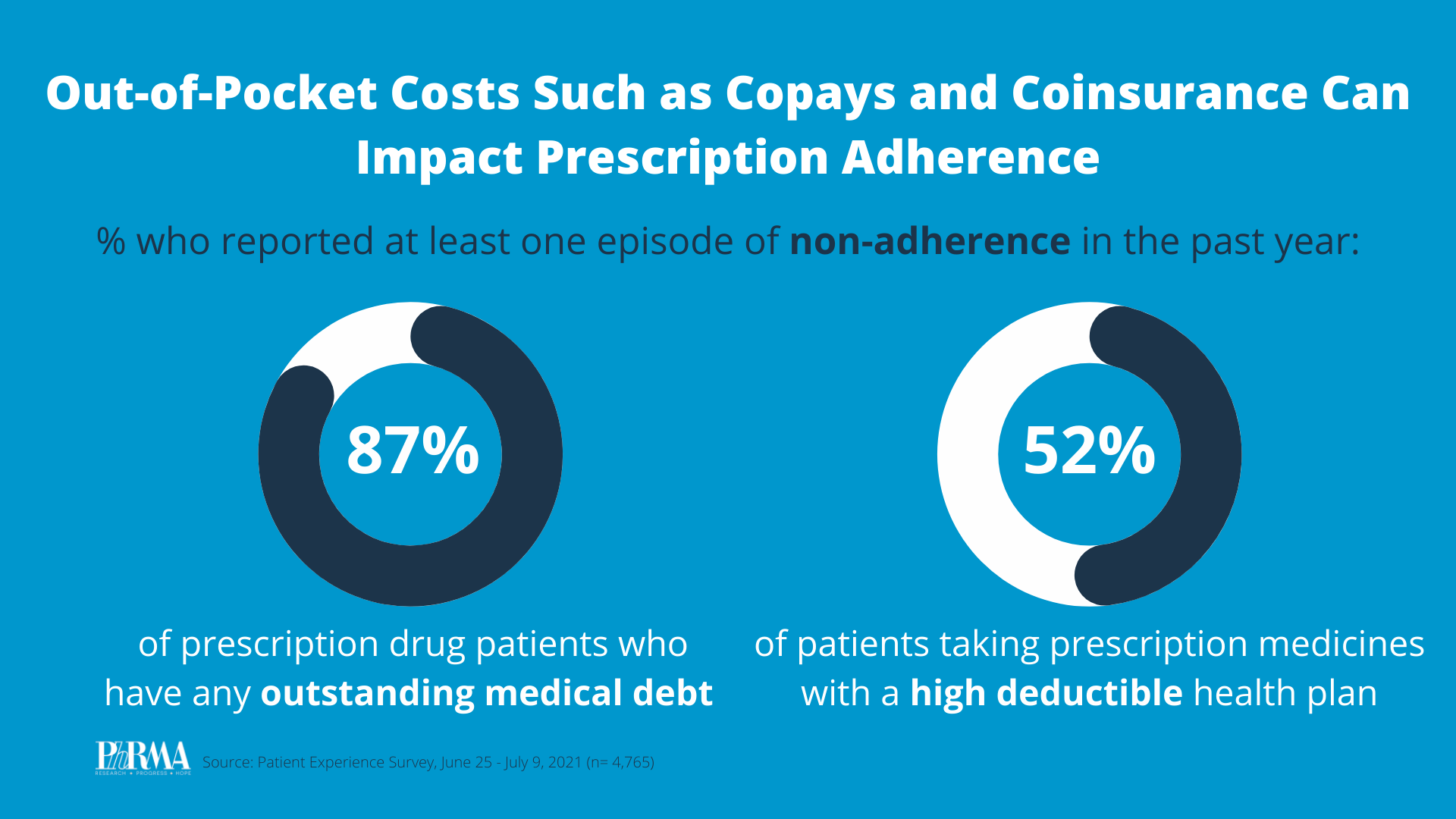
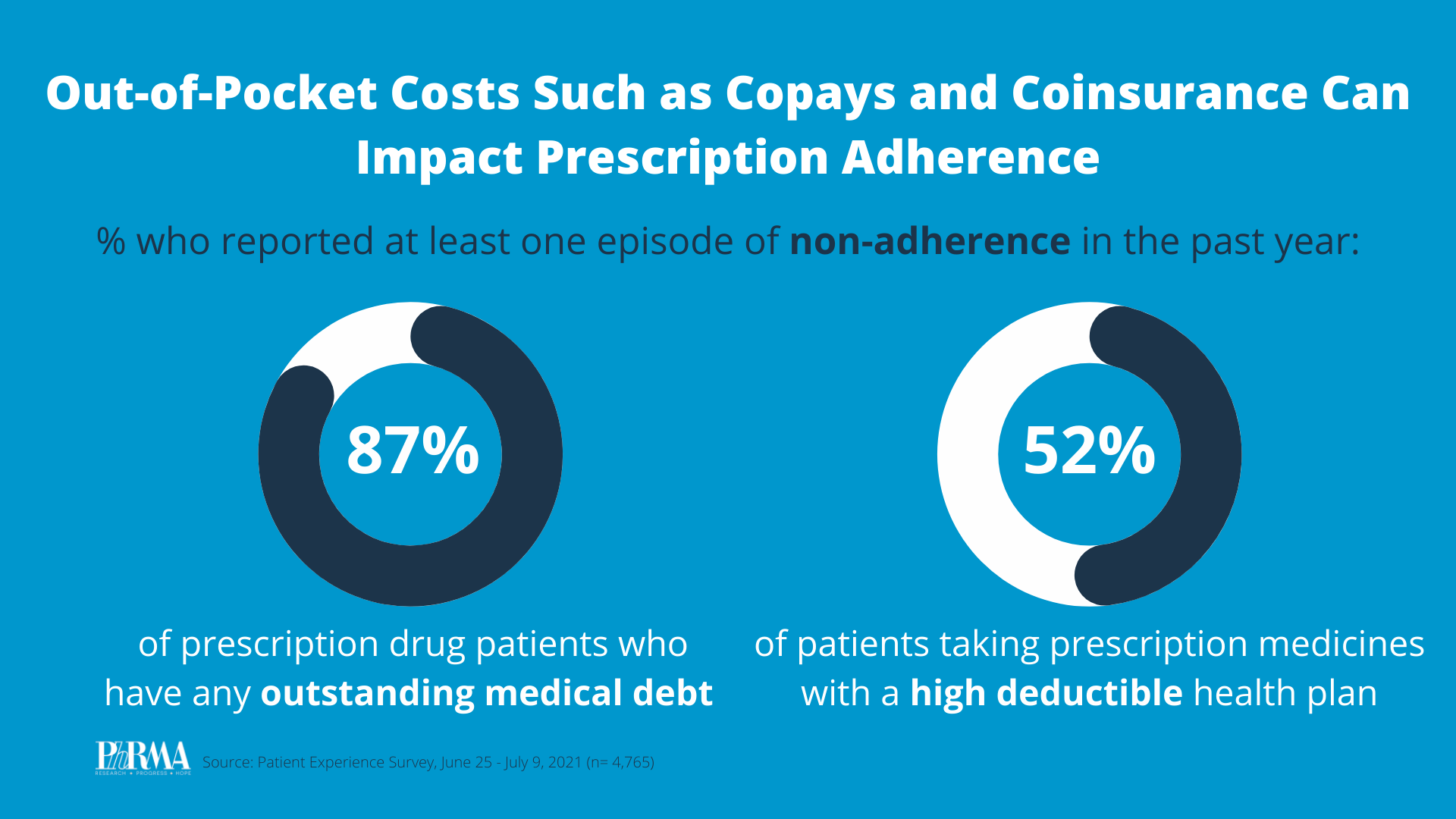
1. High out-of-pocket costs can prevent patients from accessing the medicines they need. Health insurance benefit design, which determines patients’ cost sharing, directly influences patients’ adherence to their prescription medicines. In the past year:
- 41% of patients taking prescription medicines reported at least one episode of nonadherence (not taking medicines as prescribed).
- 52% of patients taking prescription medicines in a high deductible health plan reported at least one episode of nonadherence.
- 87% of patients taking prescription medicines patients with outstanding medical debt reported poor adherence to their prescription medicines.
2. Non-adherence is most prevalent among the sickest and most vulnerable patients.
- Over the past year, patients with multiple complex and chronic conditions were more likely to report nonadherence to their treatment (46%) compared to other patients taking prescription medicines (41%).
- 55% of patients with an infectious disease delayed picking up or taking their medicine, compared with just 19% of all patients taking medicines.
- Half of patients with an autoimmune disease skipped one or more doses, compared with 27% of all patients taking medicines.
3. Non-adherence often leads to poor health outcomes and increased health care costs. Nearly half (48%) of those reporting one or more episodes of non-adherence say their health suffered as a result. Nonadherence often leads patients to require additional health services to address disease complications, that would have otherwise been prevented by medicines. For example, 85% of patients who were nonadherent to their medicines have had to seek additional health care services as a result. This is particularly evident among patients with infectious diseases: Ninety percent of patients with an infectious disease whose health was negatively impacted by poor adherence to their medication had to make another appointment with their doctor as a result.
Non-adherence to medicines and the negative health consequences is particularly troubling for vulnerable communities who already experience myriad barriers to health care access.
America’s biopharmaceutical research industry is ready to do its part to help ensure all patients can afford and access the medicines they need. Our patient-centered agenda supports making insurance work like insurance by covering more medicines from day one, making out-of-pocket costs more predictable and sharing negotiated savings on medicines with patients at the pharmacy counter.
Learn more at PhRMA.org/BetterWay.