Too many patients face high out-of-pocket costs for brand medicines, even when they have insurance.
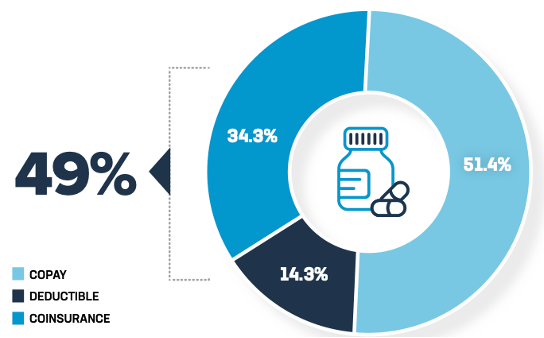
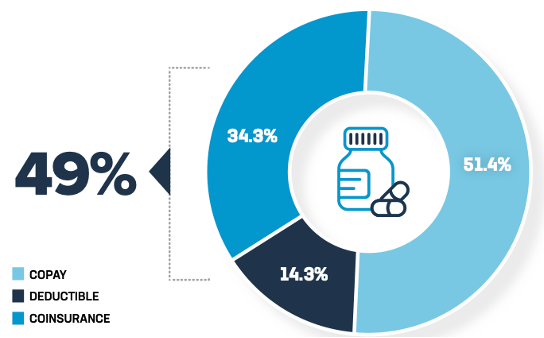
That’s because insurer-imposed barriers, like coinsurance and high deductibles, shift the cost of life-saving care onto patients. In fact, half of commercially insured patients’ out-of-pocket spending for brand medicines is based on the full list price, which may be a higher price than what their insurer paid for the brand medicine.
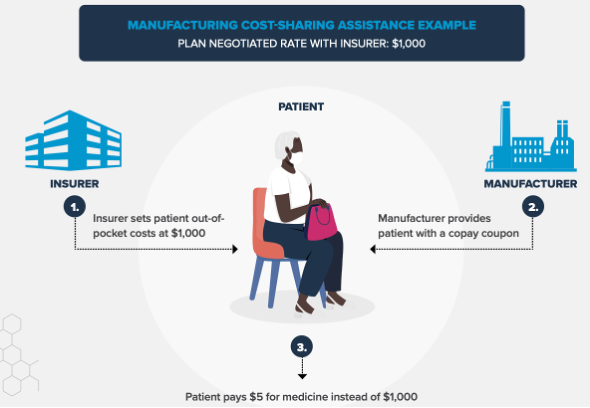
Manufacturers and others have stepped forward to assist patients with programs like cost-sharing assistance, or copay coupons. This patient assistance helps address the inadequate coverage insurers provide.
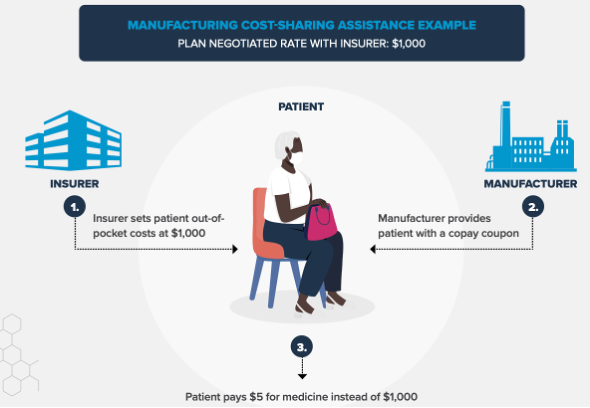
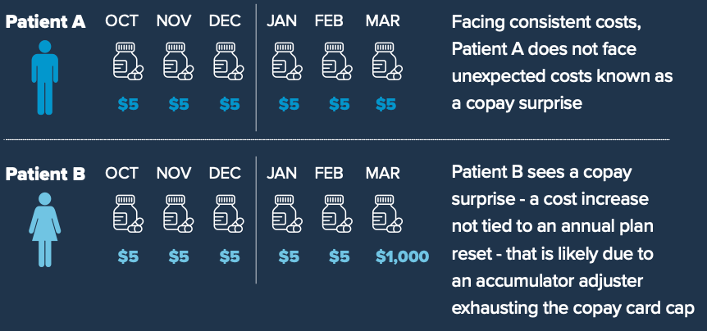
Unfortunately, insurers and middlemen known as pharmacy benefit managers (PBMs) are adopting practices that put barriers between patients and the assistance they need by barring patient assistance from counting toward deductibles and out-of-pocket maximums. These programs, known as accumulator adjustment programs, make it more likely that patients will face higher costs and abandon a prescription at the pharmacy.
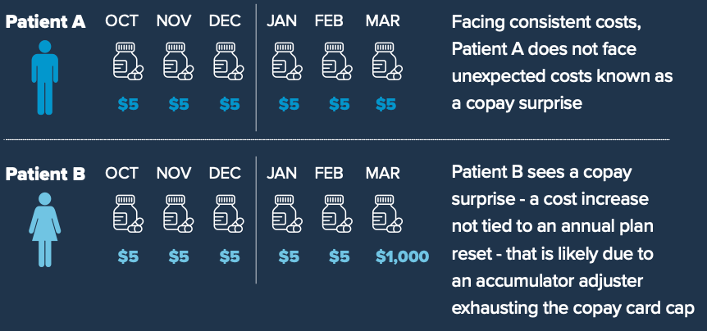
Additionally, insurers and PBMs are using other approaches called copay maximizer programs to undermine the intent of patient assistance. Copay maximizer programs often are sold to health plans by third-party entities affiliated with PBMs. They do two things:
- Target and designate specific medicines with available manufacturer cost-sharing assistance as “non-essential health benefits” so that the Affordable Care Act’s cost-sharing limitations do not apply
- Increase individual patient cost-sharing obligations to match, and therefore exhaust, the full value of the manufacturer-provided cost-sharing assistance available for those medicines
The patients who need the medicines targeted by these programs are threatened with higher out-of-pocket costs unless they enroll in the applicable manufacturer cost-sharing assistance program to access the drug. That’s not fair to patients.
Policymakers should tell insurers and PBMs to lower out-of-pocket costs by making coupons count and close policy loopholes related to coverage that allow copay maximizer programs to flourish. Read the one-pager here and learn more at PhRMA.org/Cost.