Amidst debate about rising health care costs, some policy-makers have expressed renewed interest in using cost-effectiveness thresholds as the basis for setting coverage and payment policy. But a new analysis from Xcenda shows that reliance on one-size-fits-all value assessments, such as those used by the Institute for Clinical and Economic Review (ICER), could limit hundreds of thousands of Medicare Part B beneficiaries’ access to life saving medicines.
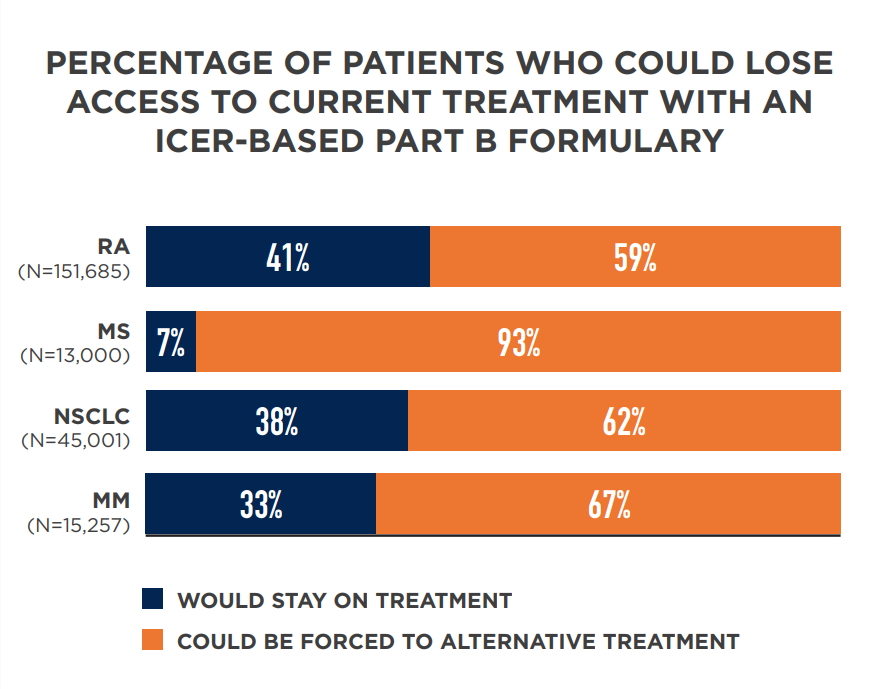
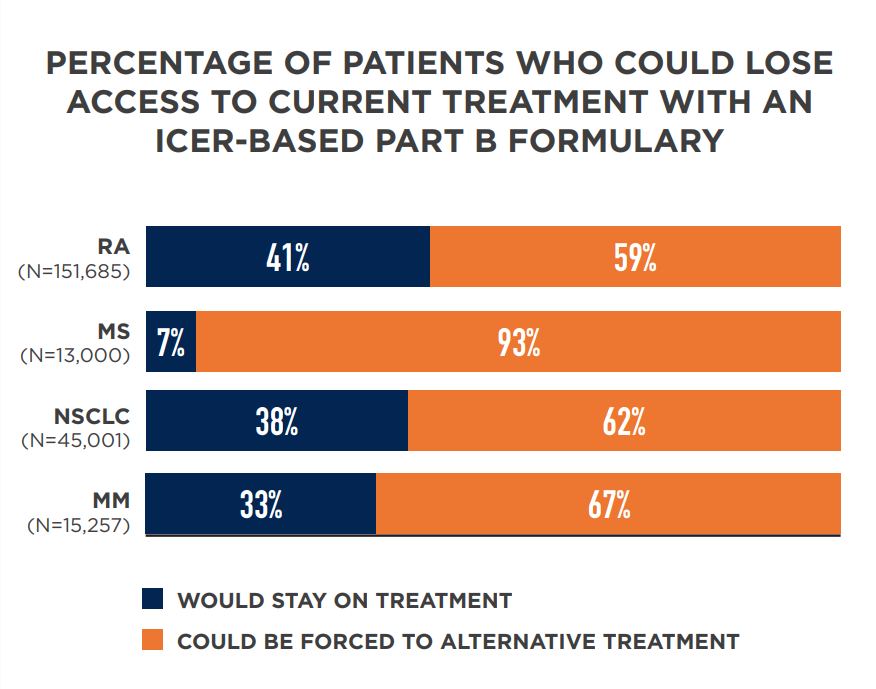
The new analysis compared ICER’s assessments regarding what treatments are of “highest value” to utilization of Medicare Part B medicines for four diseases. The data show if Medicare were to apply ICER’s determinations, which rely on cost effectiveness thresholds, as the basis for coverage policy, 62 to 93 percent of patients with rheumatoid arthritis (RA), multiple sclerosis (MS), non-small cell lung cancer (NSCLC) and/or multiple myeloma (MM) could lose access the treatments their physicians determined were best.
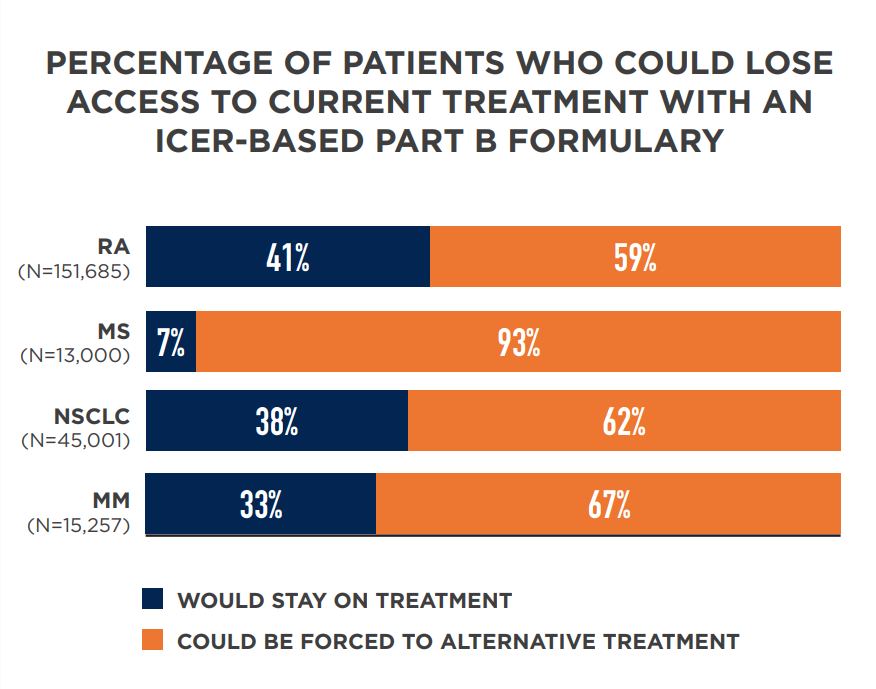
The analysis quantifies, for the first time, the profoundly negative impact using ICER’s assessments would have on Medicare beneficiaries. ICER’s framework poses particular risks for beneficiaries in part because it relies on conventional, one-size-fits-all thresholds to judge cost effectiveness. These thresholds ignore important differences in individual patient needs and preferences and have been widely criticized as discriminating against vulnerable groups such as the elderly and disabled.
Despite these concerns, some policymakers have persisted in pursuing them. For example, earlier this year the New York Department of Health began using ICER reviews and cost-effectiveness thresholds to set value-based prices for medicines in Medicaid, a move that has been sharply criticized by patient advocates. The decision by the Department of Veterans Affairs to use ICER in its coverage decisions provoked similar concern from patients, veterans and people with disabilities.
To measure the value of medicines, we need better tools that capture the complexity of the diseases and patients we treat. That is why our sector provides an unprecedented level of support to advance these tools. If we do not invest in better solutions to facilitate access to the treatments that patients value, there could be serious consequences for both patient health and progress against unmet medical need.
Read more about the Xcenda analysis here.
View the Xcenda analysis one pager here.