A new study based on IQVIA data shows alarming trends in rising out-of-pocket costs for brand medicines among Medicare Part D beneficiaries with serious and complex conditions like cancer, HIV and multiple sclerosis. The analysis, which looked at spending trends among non-low-income subsidy (non-LIS) Part D beneficiaries from 2015 to 2019 across all brand medicines and several therapeutic areas, reaffirms the need for targeted solutions to strengthen the program. Here are three findings you should know.
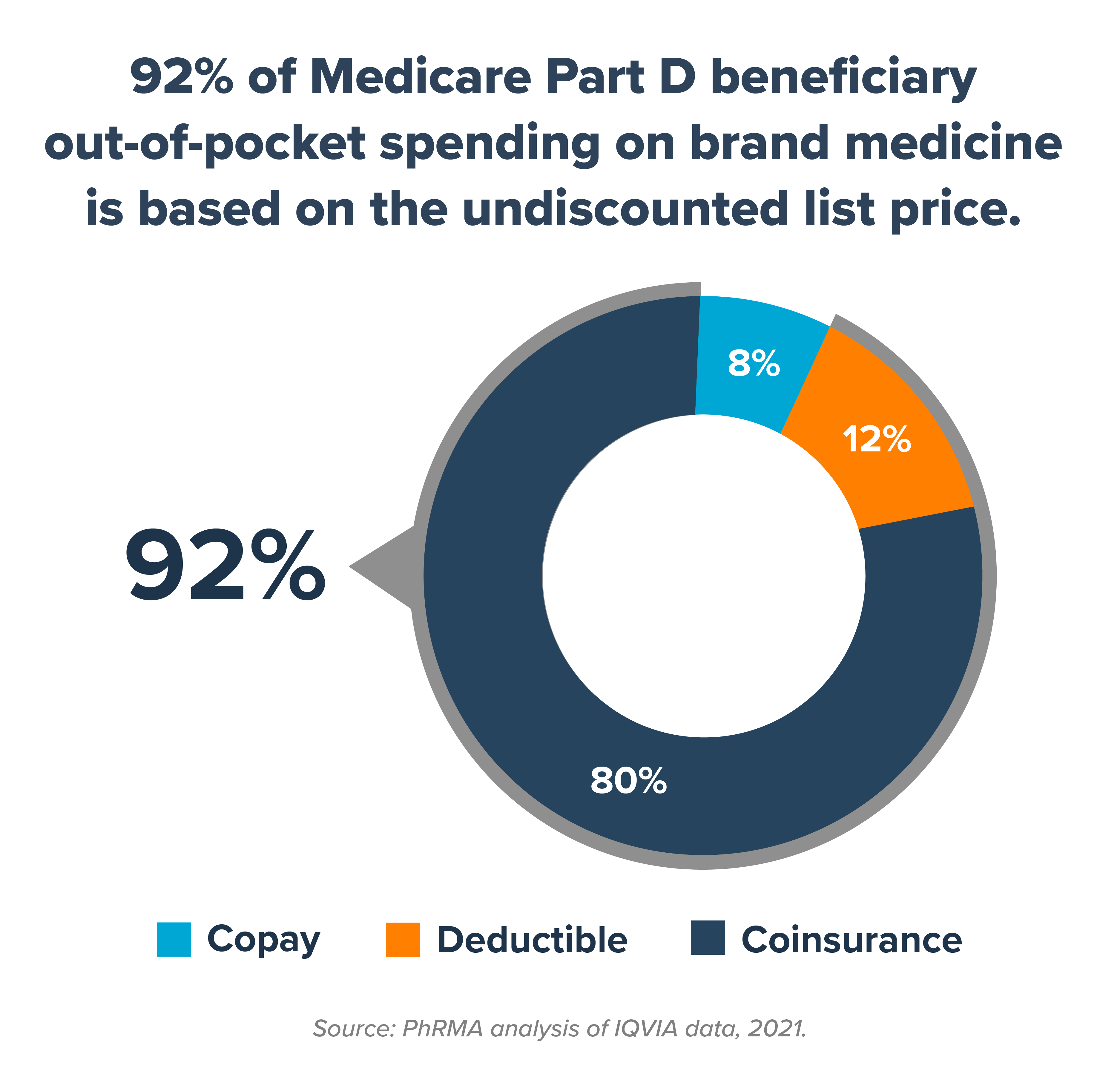
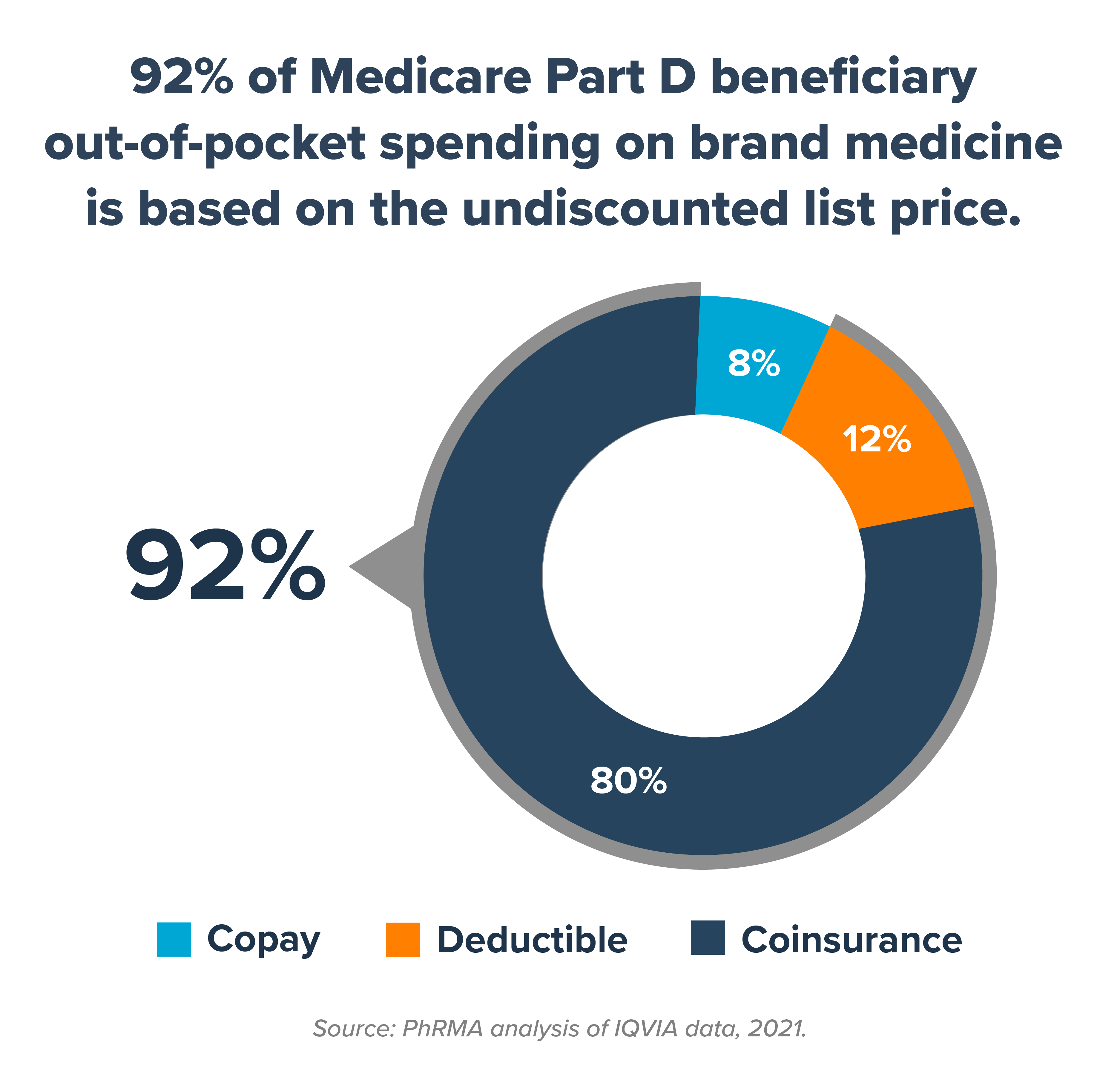
1. Coinsurance based on list price accounts for 80% of Medicare Part D beneficiaries’ out-of-pocket spending on brand medicines. Health plans and middlemen known as pharmacy benefit managers (PBMs) negotiate significant discounts and rebates with manufacturers that lower the cost of medicines. Coinsurance and deductibles, however, are typically based on a brand medicine’s full, undiscounted list price. The study found 92% of Part D beneficiaries’ out-of-pocket spending is based on the list price rather than the discounted price their insurer gets. That’s not how insurance is supposed to work.
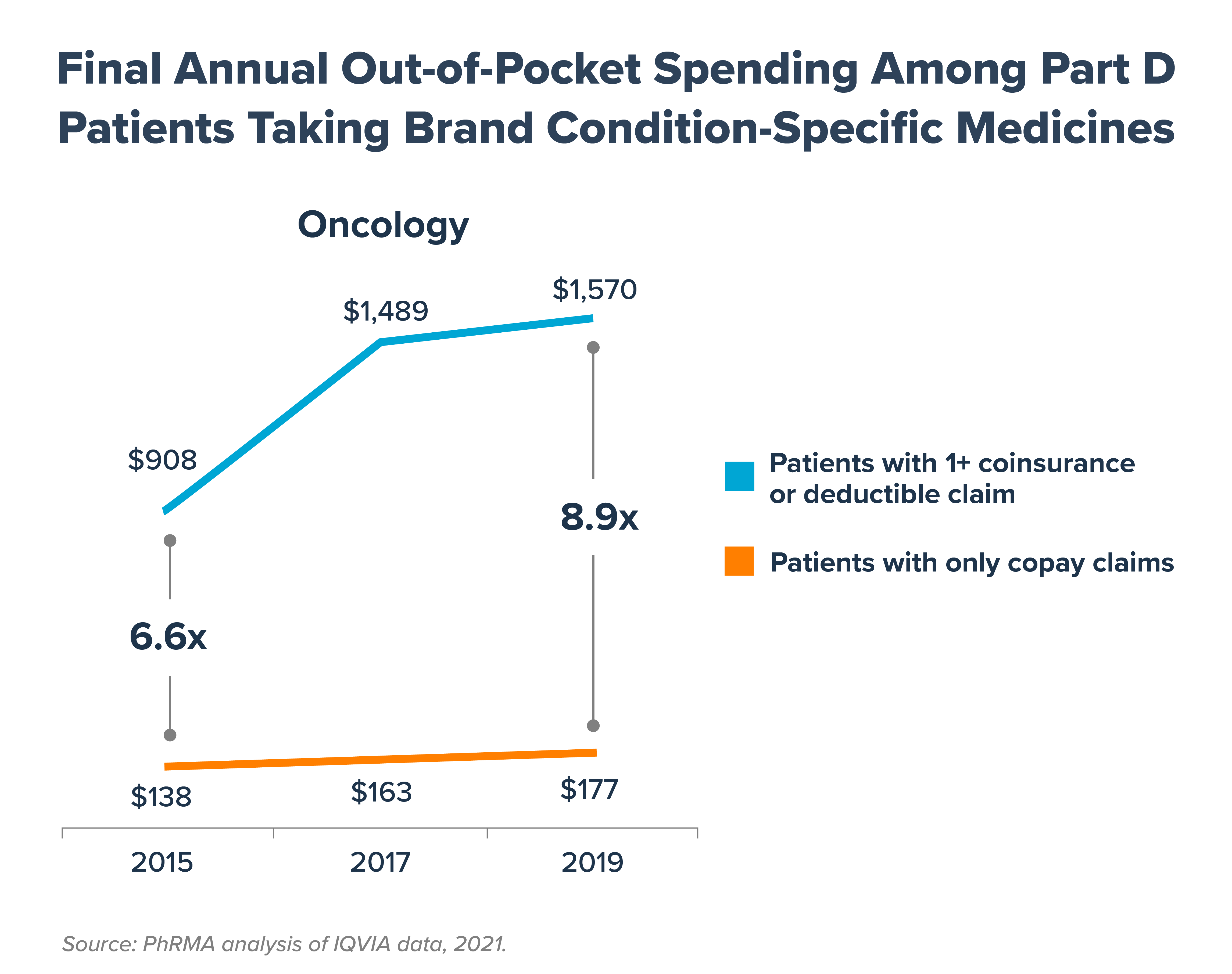
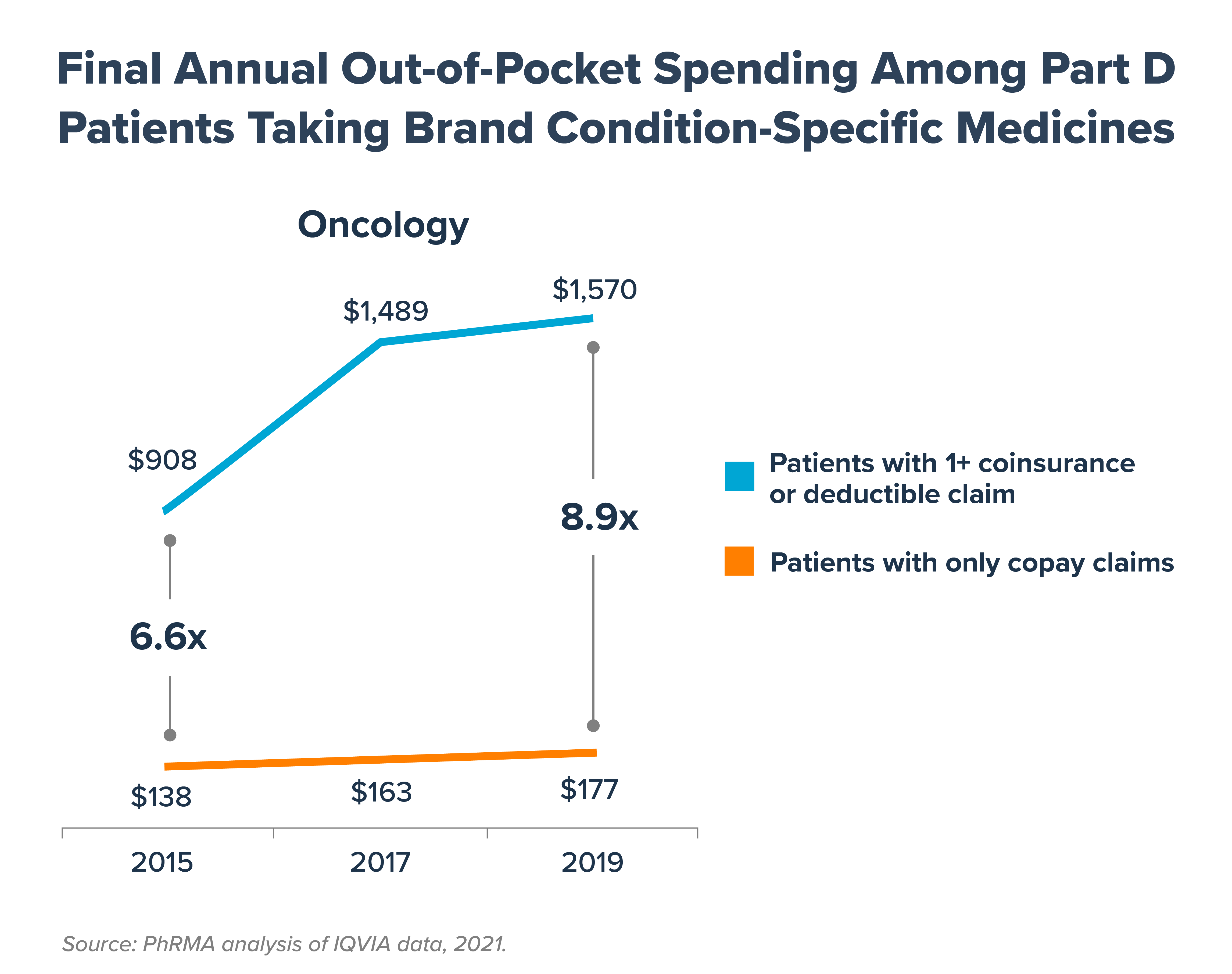
2. Average out-of-pocket spending is higher, and has grown faster, for seniors with coinsurance and deductibles. Part D beneficiaries with coinsurance and deductibles taking brand medicines for certain chronic conditions are subject to significantly higher out-of-pocket costs, on average, than those with fixed copays, and these costs are growing each year. By 2019, beneficiaries taking brand oncology medicines with coinsurance and deductibles paid 8.9 times more out of pocket, on average, than beneficiaries with only copays.
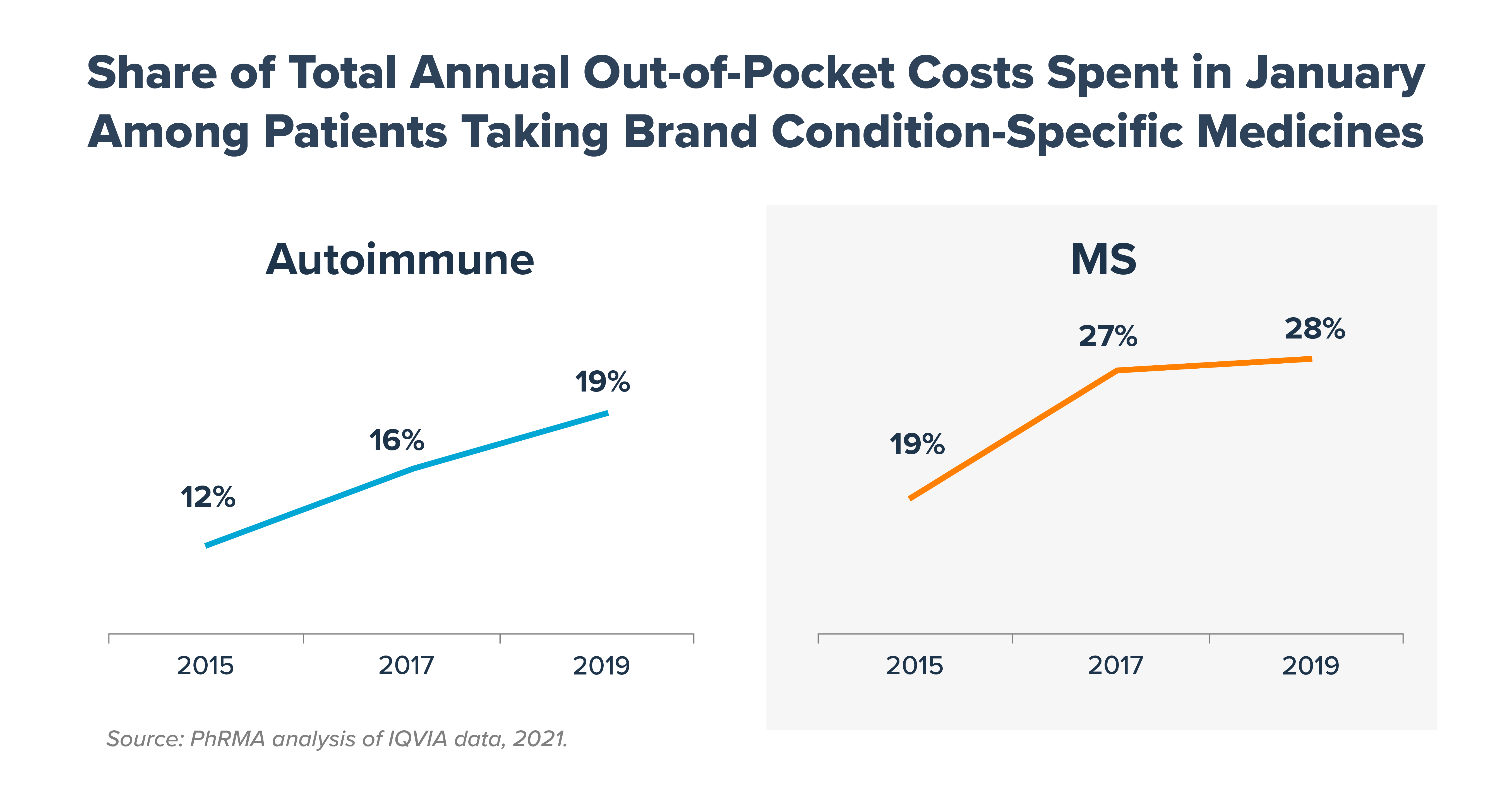
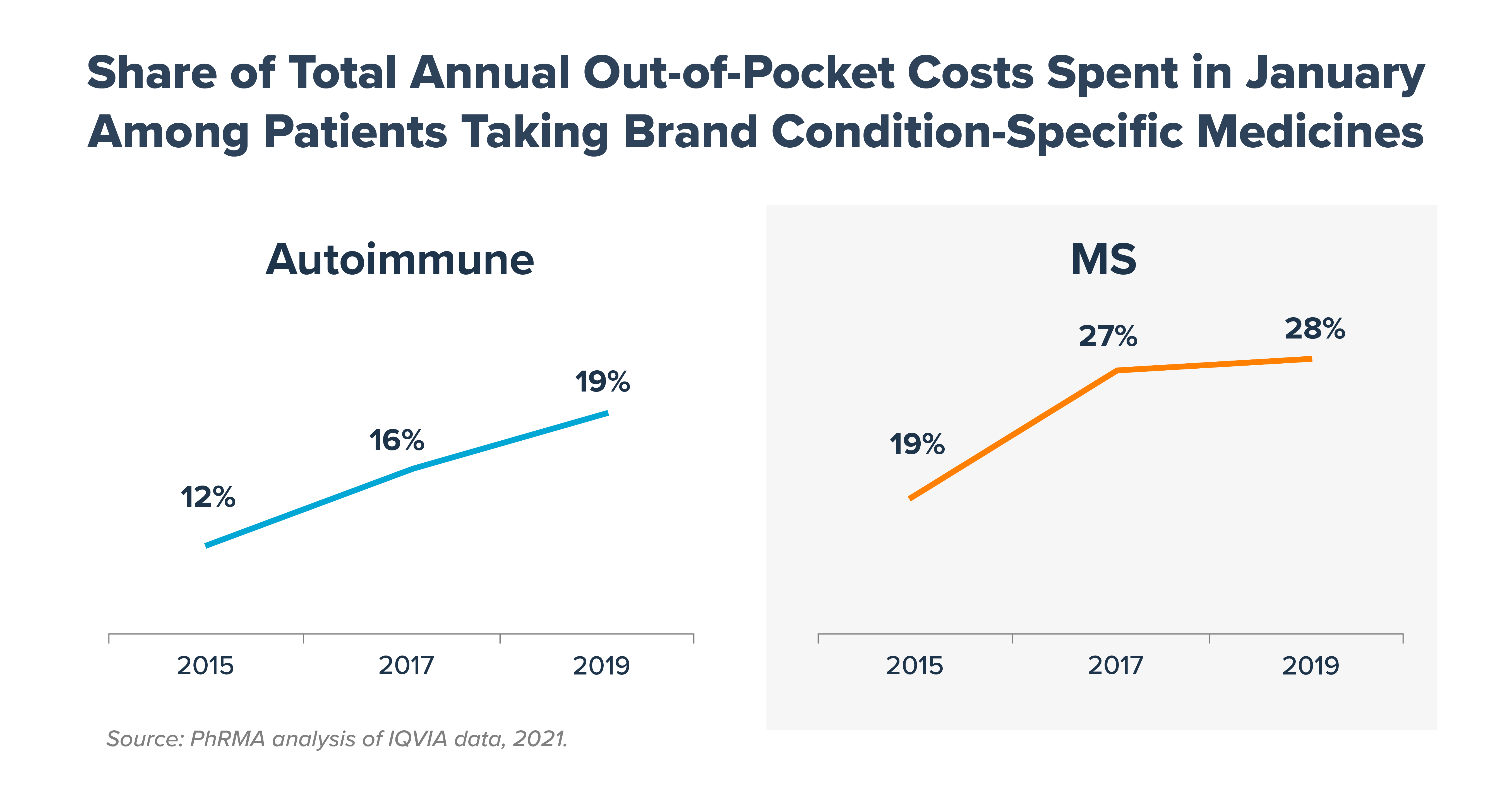
3. As plans increasingly use coinsurance, beneficiaries’ must pay a larger share of their total annual cost at the start of each year. The Part D benefit structure subjects certain Part D beneficiaries to high up-front costs at the beginning of the year. This creates serious affordability challenges. If spending were equally spread throughout the year, patients would pay 8.3% of their total annual out-of-pocket costs in the month of January. Instead, in 2019, Part D beneficiaries taking brand autoimmune medicines were responsible for nearly twice as much (19%) of their total out-of-pocket costs in January (up from 12% in 2015). Similarly, beneficiaries taking brand multiple sclerosis medicine were responsible for 28% of their total out-of-pocket costs in January (up from 19% in 2015).
These trends are further proof that health plans continue to shift medicine costs to patients with severe chronic illnesses. In order to ensure high out-of-pocket costs don’t get in the way of needed care, we need commonsense solutions that provide direct relief to patients:
- Ensuring rebates and discounts are passed on to patients at the pharmacy counter
- Capping what seniors have to pay out-of-pocket each year for prescription medicines
- Lowering coinsurance earlier in the benefit
- Spreading out-of-pocket costs throughout the year
These are precisely the kind of patient-centered, holistic changes included in “Building a Better Health Care System,” our agenda for a stronger, more resilient, affordable and equitable health care system for all. America’s biopharmaceutical research industry is ready to do its part to help ensure all patients can afford the medicines they need. To learn more, visit phrma.org/cost.