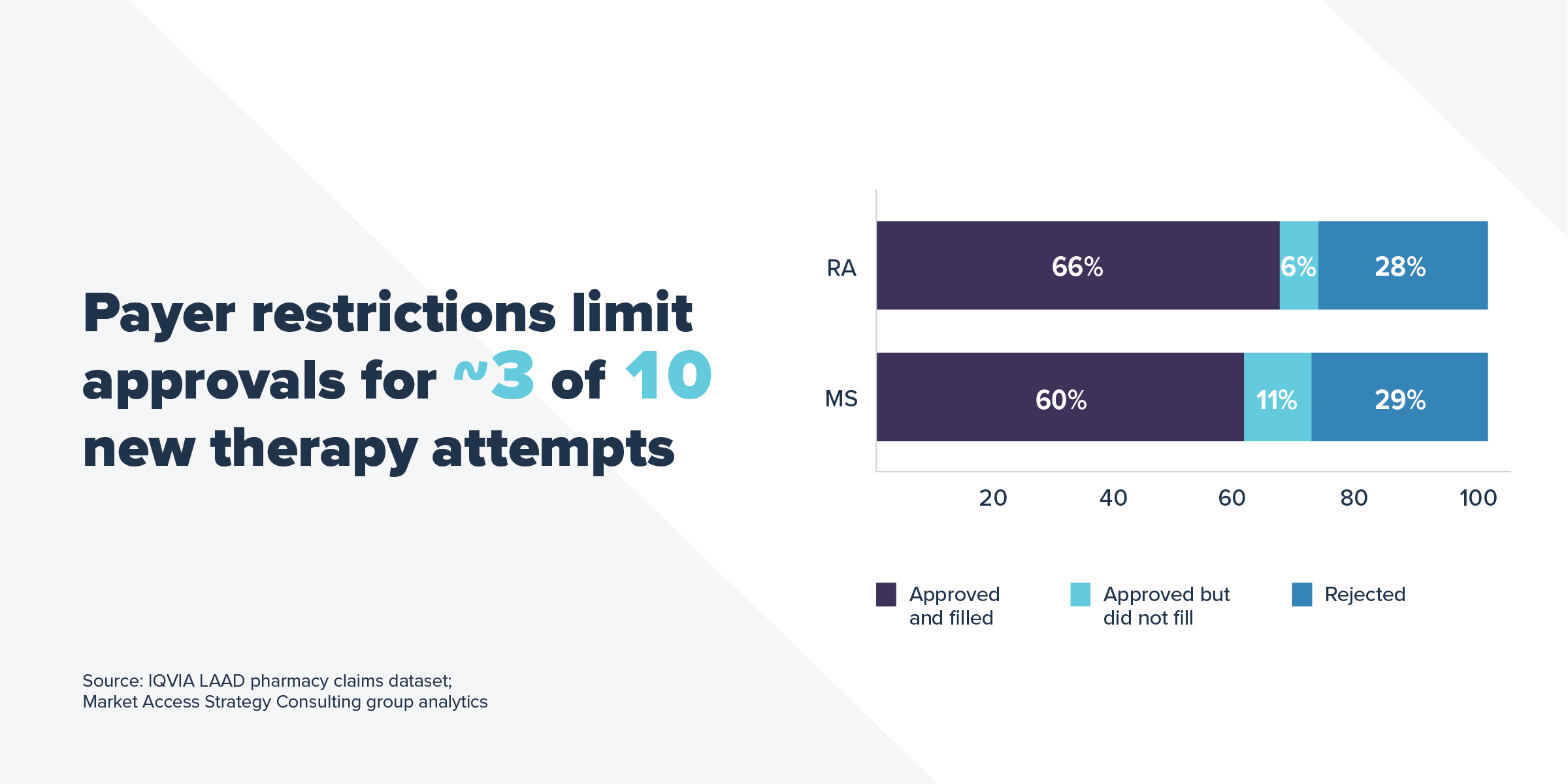
A new analysis from IQVIA shows that in 2018, 80% of commercially insured patients attempting to fill a new prescription for a rheumatoid arthritis (RA) or multiple sclerosis (MS) medicine encountered a utilization management restriction. Of those patients, 3 out of 10 were unable to gain approval from their commercial market health plan to start new treatments their doctors prescribed for them within 30 days.
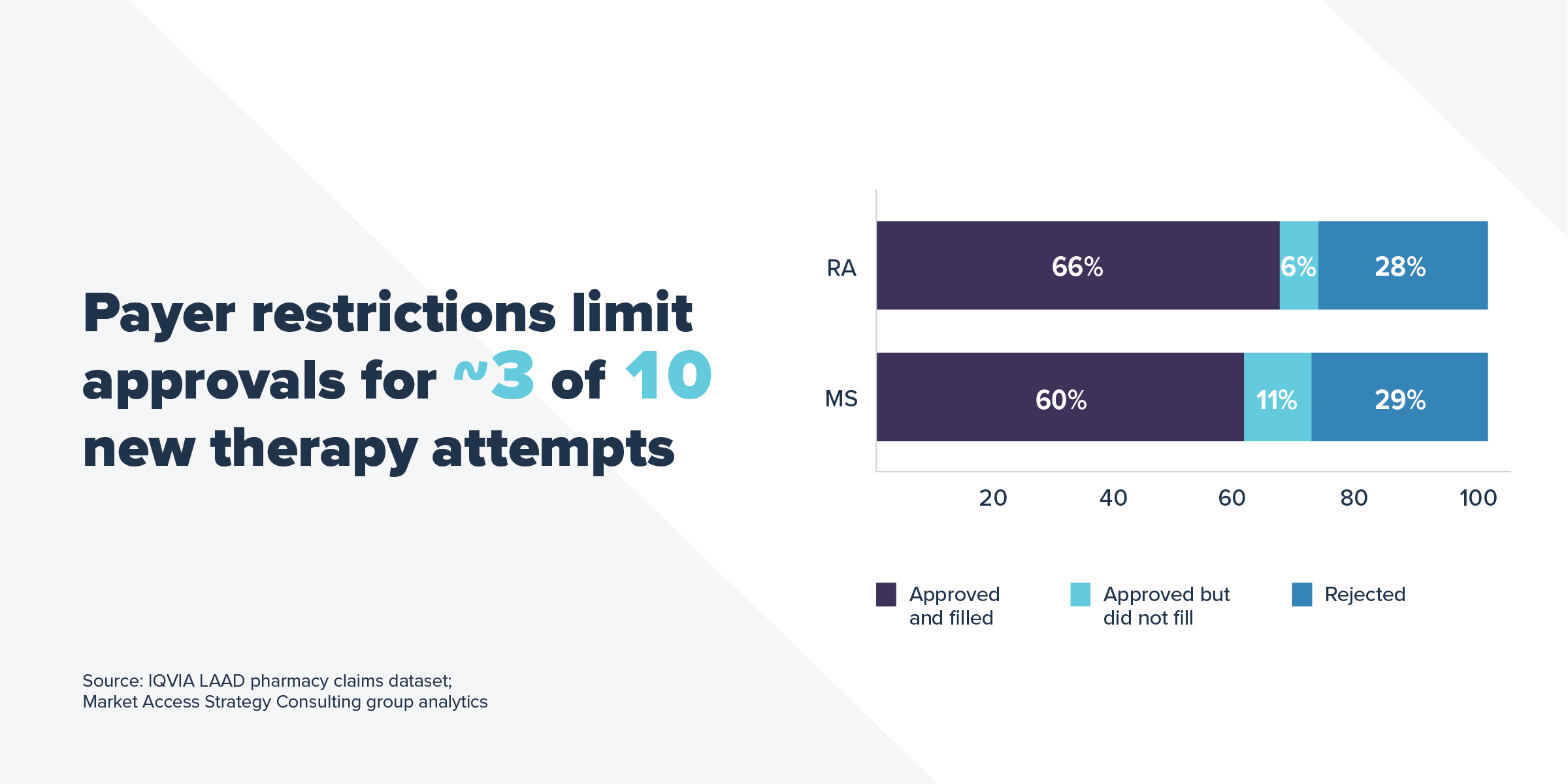
Plans have a lot of leverage to hold down medicine costs, including utilization management restrictions like prior authorization, formulary exclusions, and fail first requirements (often referred to as “step therapy”) that make a patient try certain medicines before allowing a patient to get the medicine his or her doctor originally prescribed. RA and MS patients are subjected to these restrictions at a high rate, leaving these patients more vulnerable to actions that may prevent or delay their access to medicines.
The study also found that, after meeting utilization management requirements, 60% of new commercially insured RA patients and 51% of MS patients used cost-sharing assistance to help afford their medicines in 2018. Patients facing higher out-of-pocket costs increasingly used cost-sharing assistance to help them pay for those costs, suggesting that even after satisfying plan utilization management requirements, high cost sharing may present yet another barrier to patient access.
This highlights the need for manufacturer cost-sharing assistance when payers fail to ensure that patients can access the treatments they need and not walk away from the pharmacy counter when they face high levels of cost sharing. Unfortunately, a new rule from the Administration makes it harder for patient cost-sharing assistance to count toward out-of-pocket limits to help patients pay their out-of-pocket costs for medicines. The Administration should prioritize solutions that improve patient affordability rather than allowing plans to exclude cost-sharing assistance from being counted toward patients’ out-of-pocket limits.
Learn more at www.letstalkaboutcost.org.