Did you know that insurance companies use middlemen — known as pharmacy benefit managers (PBMs) — to decide what medicines people can get and what people pay out of pocket for those medicines?
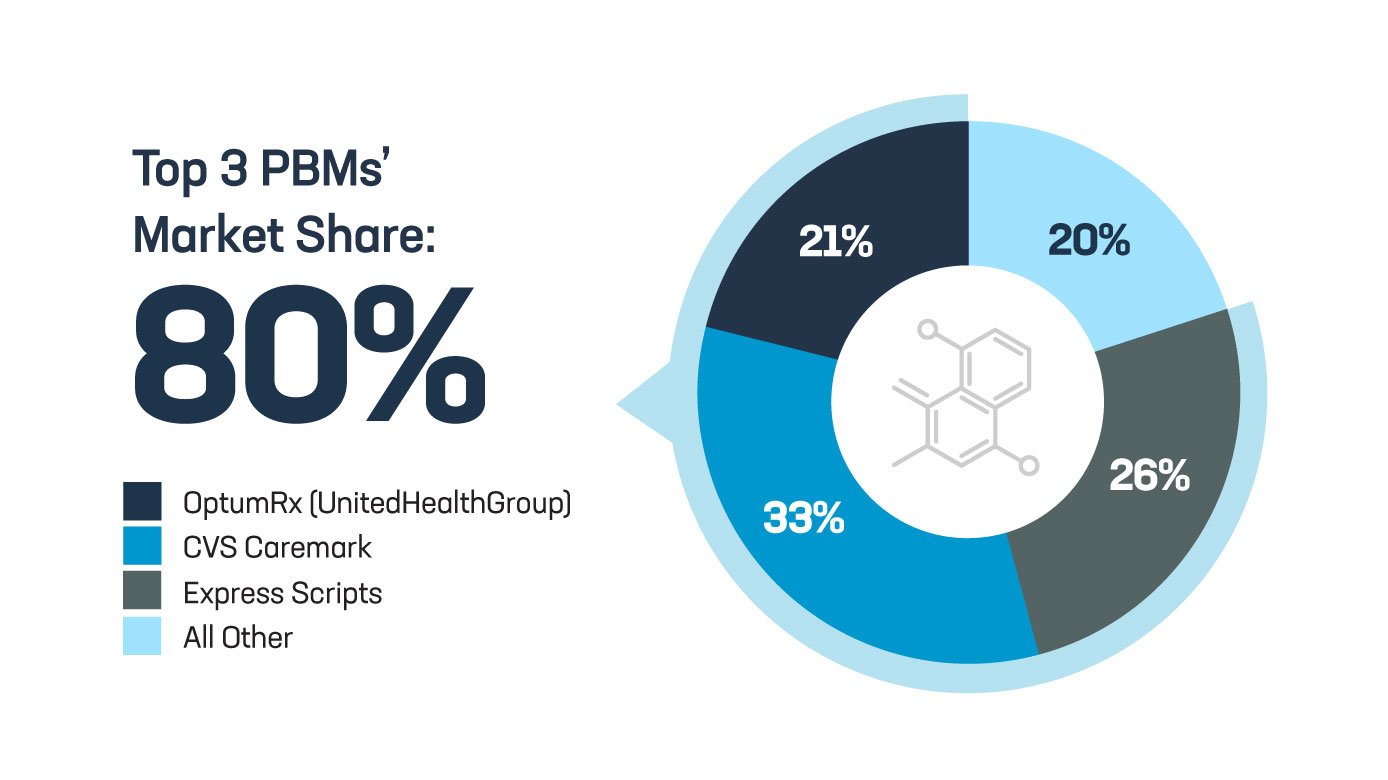
These middlemen operate in a black box with little transparency and accountability, with the top three PBMs controlling 80% of the entire prescription drug market.
A hearing in the Senate’s Commerce, Science and Transportation Committee will dive into these and other important issues, and senators on both sides of the aisle will discuss ways to bring greater accountability to the PBM industry.
PBMs profit off a business model rife with conflicts of interest and engage in tactics that can drive up costs and make it harder for patients to get their medicines. Before this morning’s hearing kicks off, here are a few PBM tactics that merit congressional oversight:
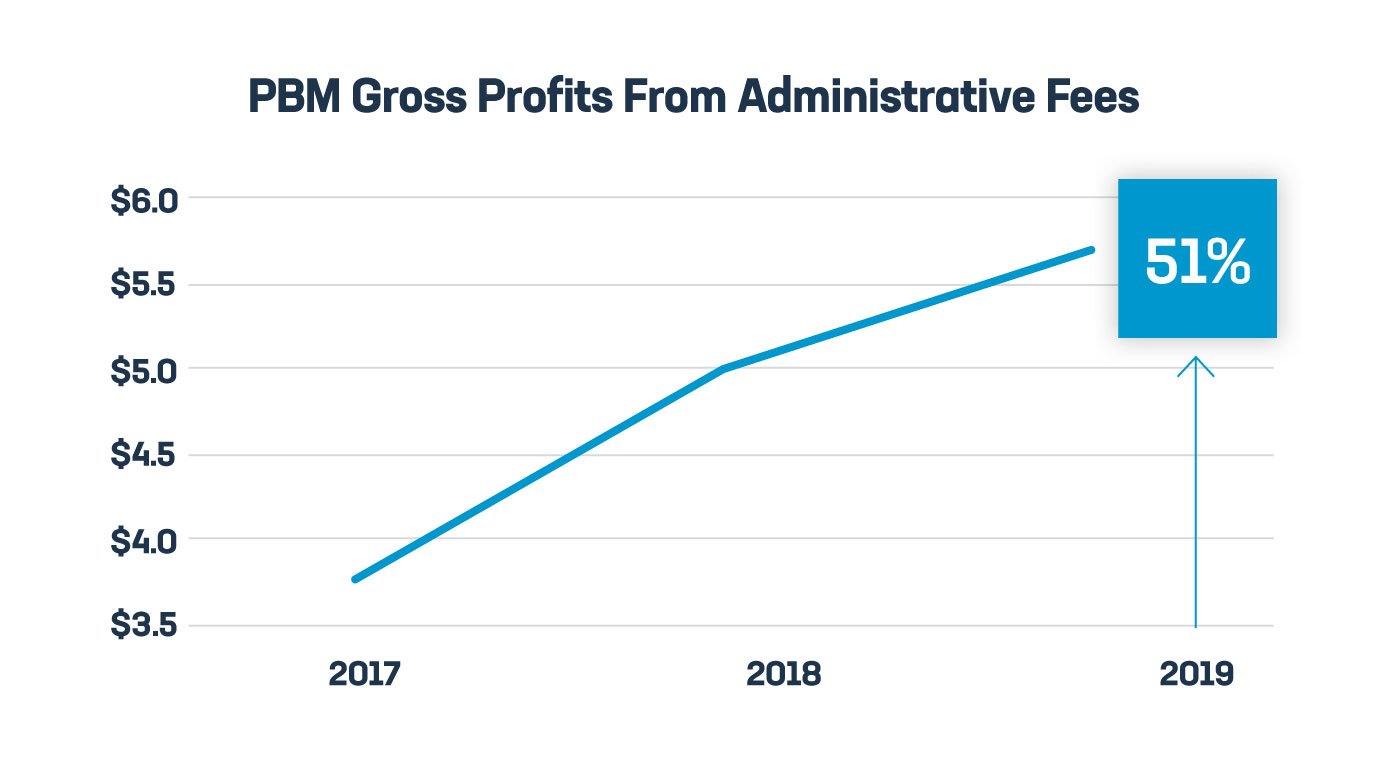
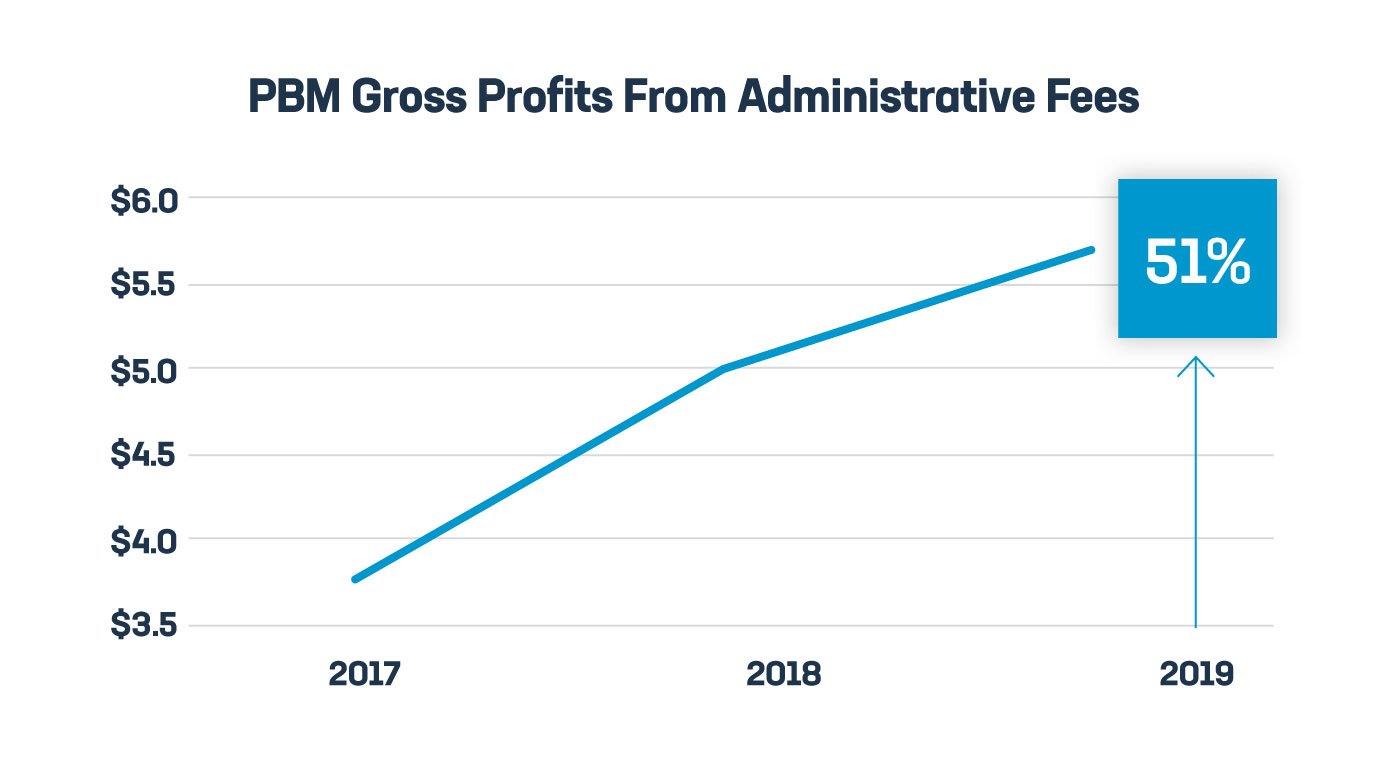
- Fees tied to prices. Middlemen extract rebates and fees tied to the price of medicines, and this has allowed PBM profits to soar, up nearly 51% from just a few years ago. But experts warn it can also lead to higher costs for patients at the pharmacy. These practices are under increasing scrutiny by states, Congress and federal regulators.
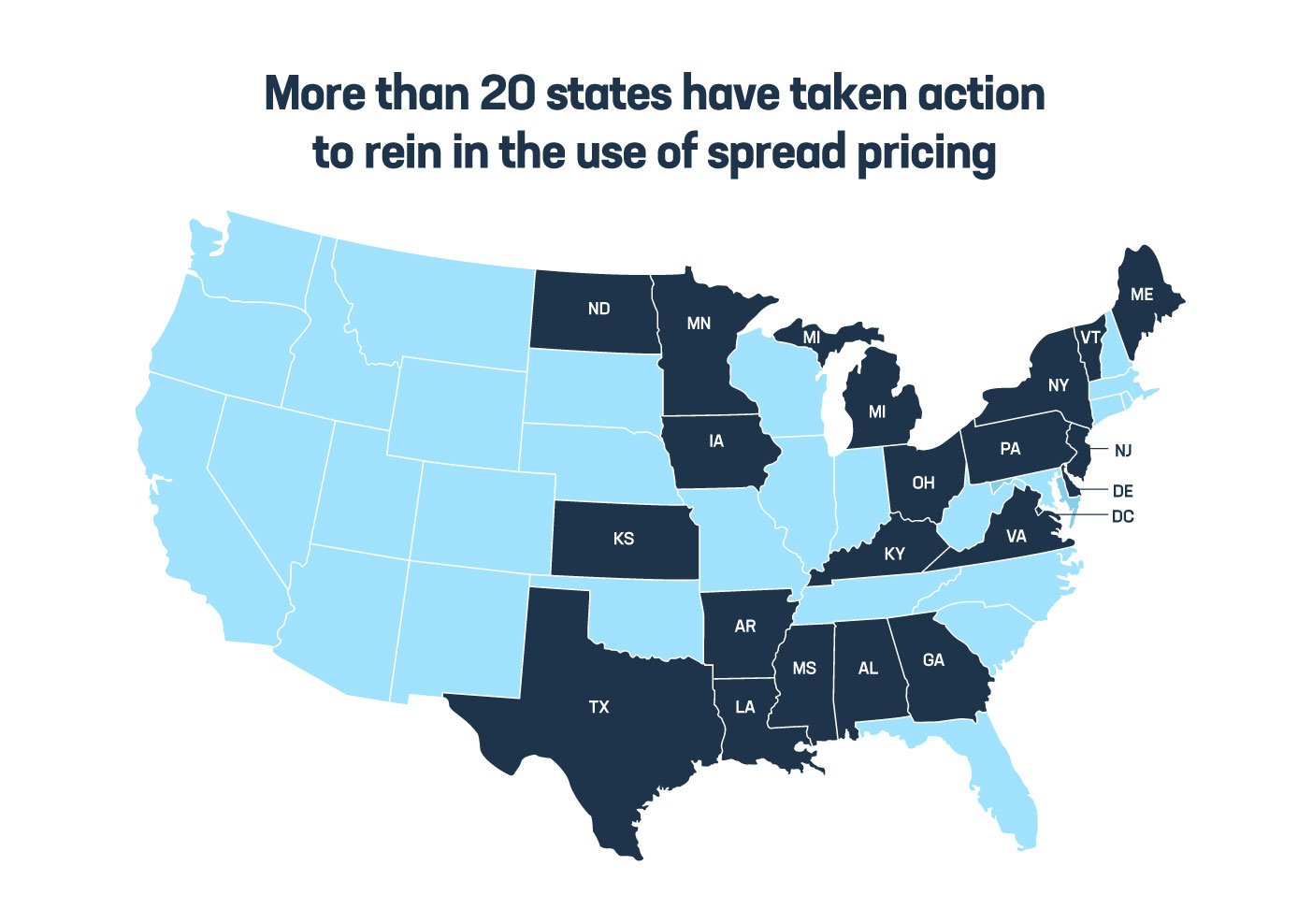
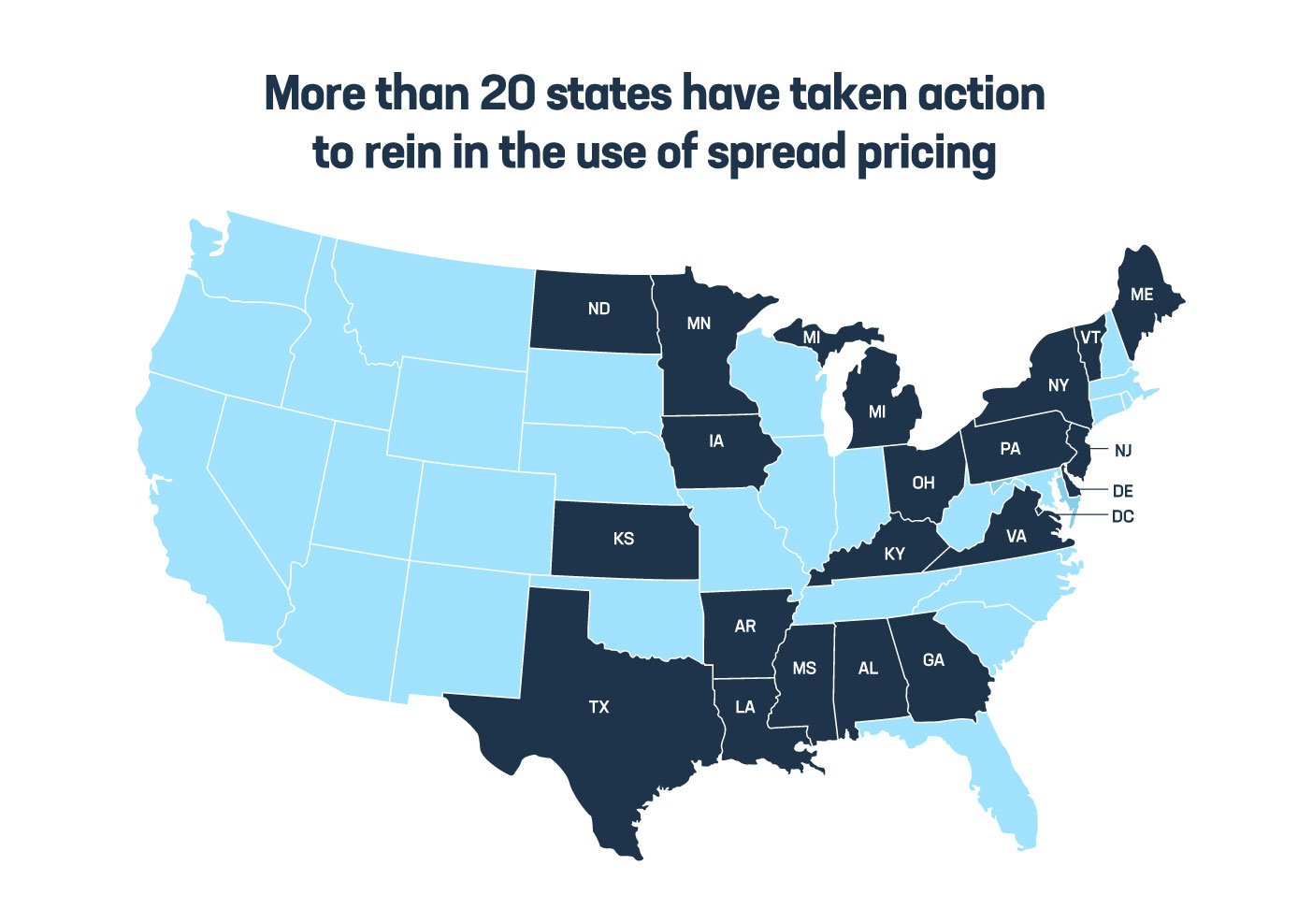
- Spread pricing. PBMs often bill health plans, employers and government health programs more than what they pay to the pharmacy for medicines and pocket the difference. For example, the state of Ohio was overcharged nearly $225 million in a single year due to PBM spread pricing. More than 20 states have taken action to rein in spread pricing, and prohibiting the use of spread pricing in Medicaid would save taxpayers an estimated $900 million over 10 years.
- Patient steering. PBMs increasingly required patients to pick up their prescriptions at pharmacies the PBM owns or has another financial relationship with. This can include a retail pharmacy, mail-order pharmacy or specialty pharmacy. According to one survey, more than 75% of community pharmacists said their patients’ prescriptions were steered toward another pharmacy without their patients’ knowledge or consent.
By demanding more accountability, Congress can rein in these abusive practices and provide meaningful relief to patients and taxpayers. There are important steps lawmakers must take to hold these middlemen accountable:
- Break the link between fees and price. Require that PBMs receive a flat fee for their services that isn’t based on the price of a medicine, strengthening incentives for middlemen to choose medicines that lower costs for patients.
- Prohibit spread pricing. Save money for patients and taxpayers by ensuring health plans, employers and government programs are getting the best deal possible.
- Rein in patient steering. Help patients get the medicines their doctors prescribe at a pharmacy that’s convenient for them, not one that pads the profits of PBMs.
- Demand greater transparency. Require full disclosure of the aggregate rebates, administrative fees and other payments PBMs receive so stakeholders fully benefit from negotiated savings.
To learn more, visit PhRMA.org/Middlemen.