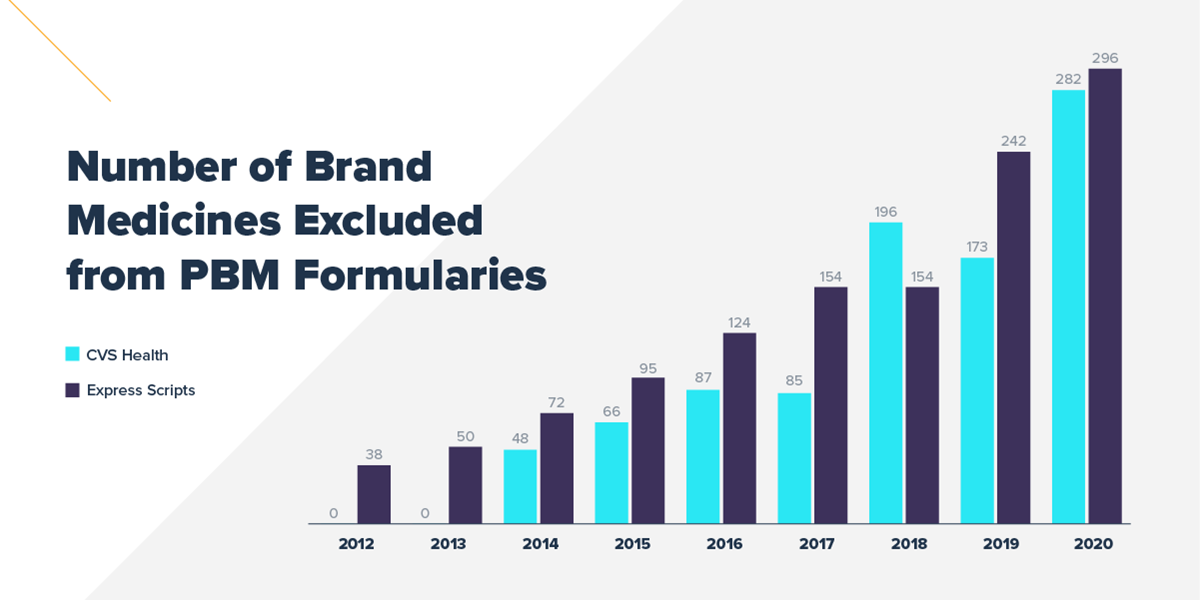
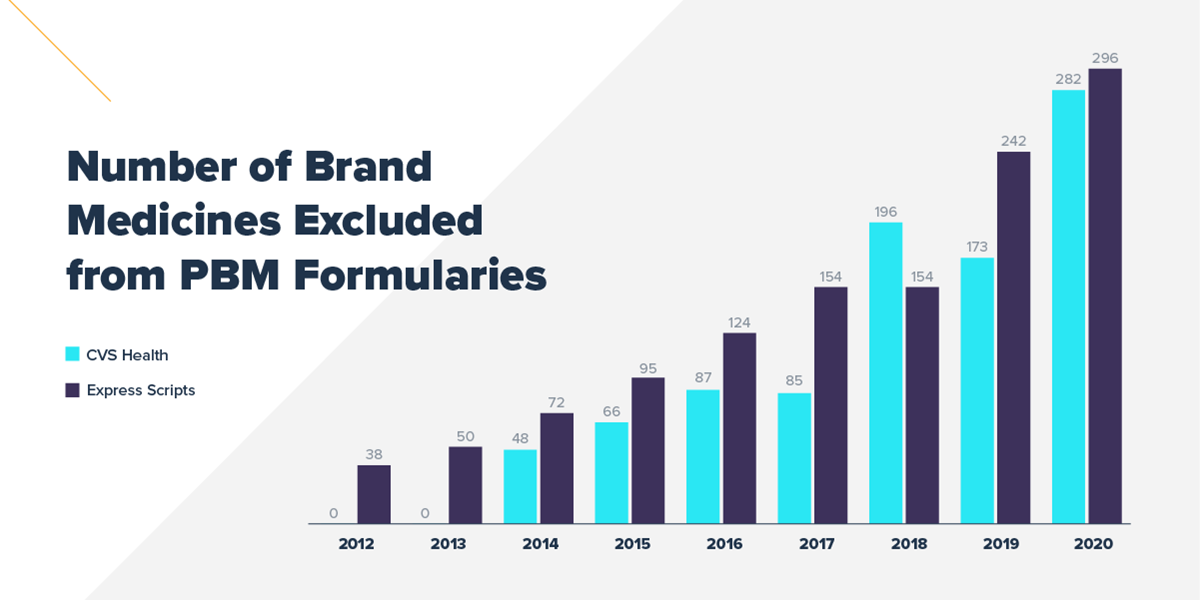
The two largest pharmacy benefit managers (PBMs), CVS Caremark and Express Scripts, have once again increased the number of medicines on their standard formulary exclusion lists. Medicines excluded from formularies treat many chronic and complex conditions, including depression, diabetes and multiple sclerosis. As these PBMs control over half of the market combined, these changes have widespread implications for patients across the country.
- CVS Caremark increased the number of excluded medicines by 109, bringing the total number of medicines excluded from their 2020 formulary to 282
- Express Scripts increased the number of excluded medicines by 54, bringing the total number of medicines excluded from their 2020 formulary to 296
- From 2017 to 2020, CVS Caremark and Express Scripts increased the number of medicines excluded from their formulary by 88% and 208%, respectively
PBMs leverage their vast purchasing power and ability to exclude medicines from their standard formularies to negotiate large rebates and discounts from biopharmaceutical companies. PBMs then compel insurers and employers to use standard formularies by reducing the rebates offered to those who choose to adopt custom formularies without exclusions, which increases costs to the plan sponsor. In 2019, manufacturer rebates, discounts, fees and other price concessions grew to $175 billion. However, these rebates and discounts are typically not shared with patients at the point-of-sale.
Formulary exclusions can create additional barriers for patients who may experience challenges accessing prescribed treatments. These barriers to access can lead to health complications resulting from delayed treatment initiation or treatment disruption.
While PBMs increasing the number of medicines excluded from their formularies is nothing new—both CVS Caremark and Express Scripts have increased the number of excluded medicines annually since the practice began—in a time when the COVID-19 pandemic is creating new challenges for patients, PBMs should prioritize patient access, not creating more barriers.
To help patients in this time of increased financial insecurity, PhRMA member companies are expanding their assistance programs to help more people. Learn more about these resources by using the Medicine Assistance Tool (MAT).