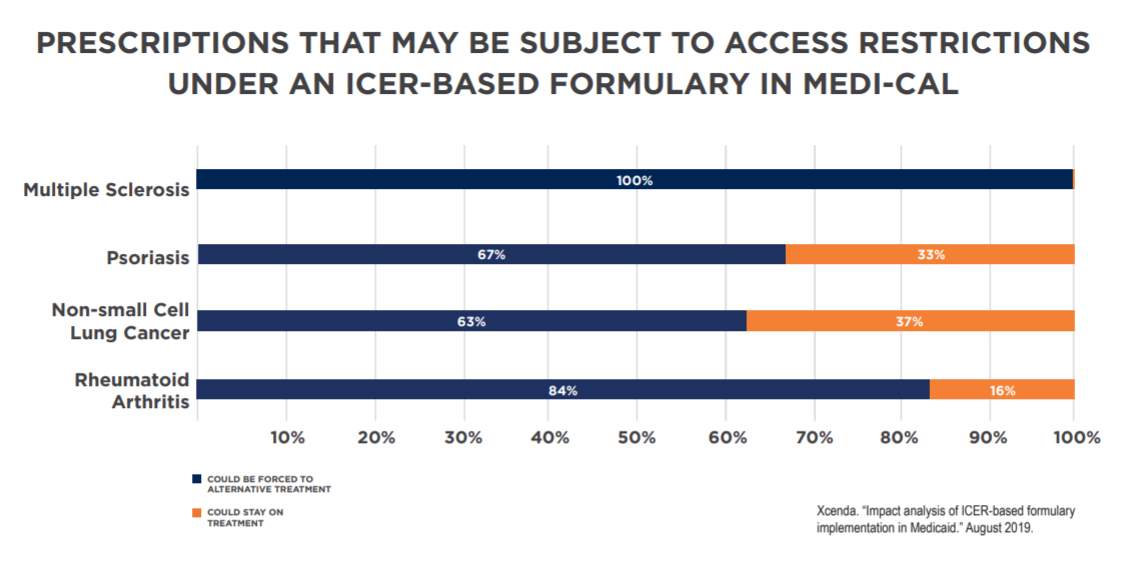
A new analysis from Xcenda applied the Institute for Clinical and Economic Review’s (ICER) value assessments to state Medicaid programs in California, Massachusetts, Maryland, Nevada and New York. The study found these one-size-fits-all value assessments could prevent or delay access to prescriptions to treat serious, complex conditions like multiple sclerosis (MS), rheumatoid arthritis (RA), non-small cell lung cancer (NSCLC) and psoriasis.
This study builds on a nationwide look at Medicaid, which found cost-effectiveness thresholds would change access to more than 820,000 prescriptions for medicines that treat some of the most vulnerable patients across the country. For example, the study found that if Medi-Cal – California’s Medicaid program – used an ICER-like standard, 73,666 prescriptions per year could face restrictions.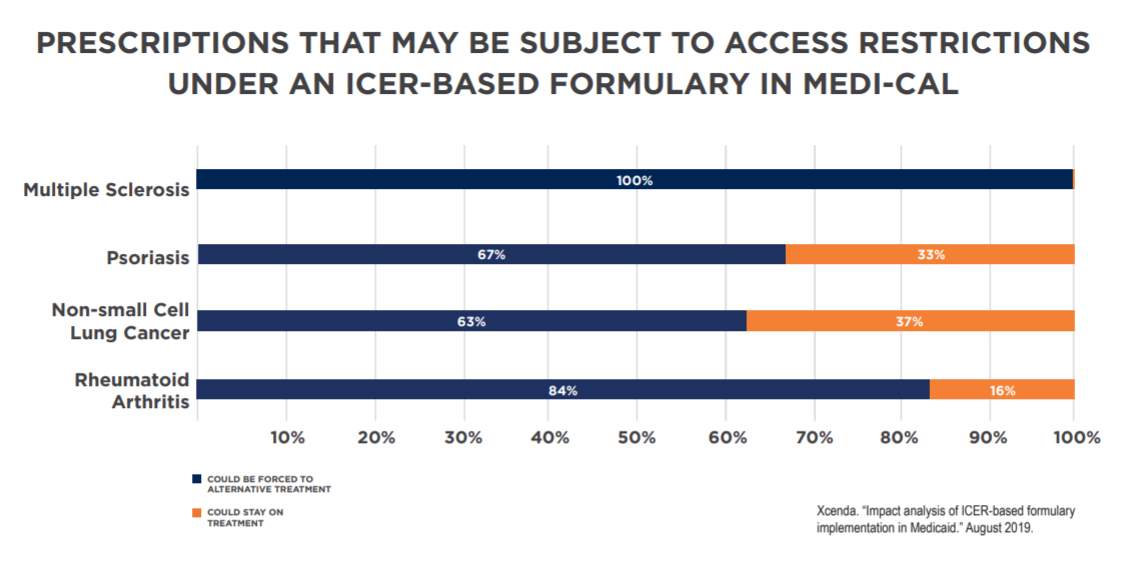 While exceptions and appeals processes in each state could reduce the impact of an ICER-based formulary, they have been shown to add burden to health care providers and patients, resulting in delayed access to treatments.
While exceptions and appeals processes in each state could reduce the impact of an ICER-based formulary, they have been shown to add burden to health care providers and patients, resulting in delayed access to treatments.
Changing how Medicaid works through value assessments like those conducted by ICER could have serious implications for patients. For example, states have recently proposed that they have flexibility to exclude new drugs from its Medicaid formulary based on value assessments, which are based on what’s best for the “average” patient, and undervalue the lives of seniors, people with disabilities and patients with chronic diseases. Because value assessments undervalue their lives, this policy could prevent access to much needed medicines, leading to worse outcomes and increased costs. Giving states the flexibility to use discriminatory methods to determine coverage and access to medicines in Medicaid would open the door to this type of standard in other programs at the federal level.
While value assessments are an important tool in moving toward a value-based health care system, it is also important that they take into account all the outcomes that matter to patients and families, including caregiver burden and the ability to work and care for one’s family. ICER’s framework takes the wrong approach, ignoring what matters most to patients and interfering with doctor-patient relationships.
Read more about the Xcenda analysis here.
View the Xcenda analysis one pagers by state here:
California | Massachusetts | Maryland | Nevada | New York



 While exceptions and appeals processes in each state could reduce the impact of an ICER-based formulary, they have been shown to add burden to health care providers and patients, resulting in delayed access to treatments.
While exceptions and appeals processes in each state could reduce the impact of an ICER-based formulary, they have been shown to add burden to health care providers and patients, resulting in delayed access to treatments.