This weekend marked the start of the annual meeting of The American Society of Clinical Oncology (ASCO). This year’s meeting, which features a theme of “Innovation and Illumination,” highlights the exciting progress we’re making in treating cancer, as well as the growing interest in new “value-based payment models in cancer care. In the midst of these discussions, new research released by Avalere Health points to the critical importance of ongoing work to close gaps in cancer quality measures in order to advance these new payment models.
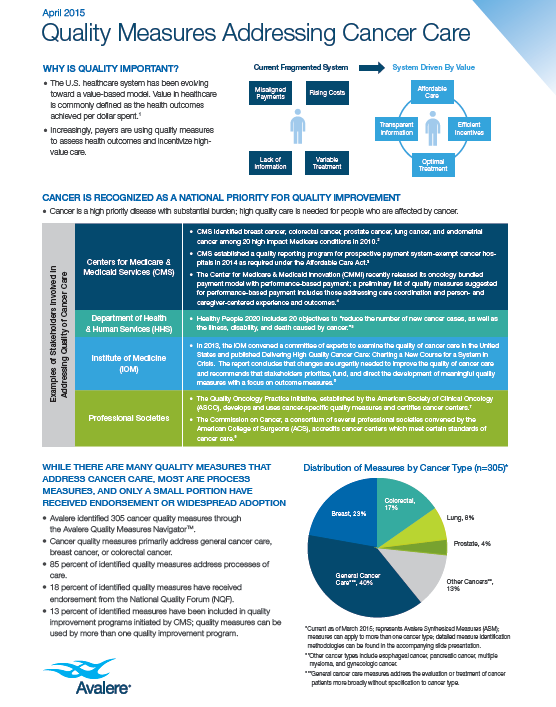
The Center for Medicare & Medicaid Services (CMS), ASCO, and other key stakeholders are actively engaged in the development and testing of value-based payment models for cancer care with the goal of improving quality and reducing costs. Several organizations have identified cancer as a national priority for quality improvement. However, measuring quality in cancer is challenging. Scientists now recognize cancer as a set of over 200 unique diseases, the treatment of which can include multiple phases, modalities, and combination strategies. Avalere analyzed 305 different cancer quality measures and found that even with the volume of available measures, gaps remain.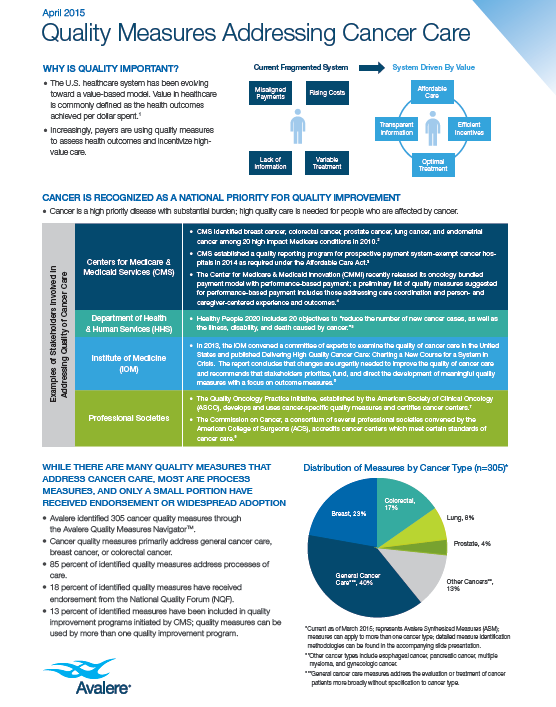
The dearth of outcome measures for cancer is one of the most notable gaps identified by Avalere. Of the measures studied, 85 percent assess process of care, meaning whether or not care follows established guidelines. Very few of the available measures addressed the clinical or patient reported outcomes of care provided, like functional status, patient experience, and quality of life. Additional measure gaps included care coordination, patient adherence, survivorship care, and management of comorbidities.
Clinical practice guidelines represent one key building block, but not the only one. If we want to pay for cancer care that patients value, we need to measure and reward what they value. This includes considering a patient’s individual preferences, characteristics and treatment goals. Patients must be at the core of our quality measurement approach, and stakeholders from across the health care landscape need to be involved in the development of measures that capture quality of care from the patient perspective. It might not happen overnight, but we must collaborate and work quickly – the quality of cancer care is at stake.
PhRMA is committed to working with stakeholders across the cancer community to accelerate progress against cancer and foster high-value, patient-centered cancer care. Working to ensure we have sound quality measures in place is just one part of this.
Get instant updates on issues you care about - here. {{cta('4fe14269-44de-493b-a19c-946e0454614a')}}