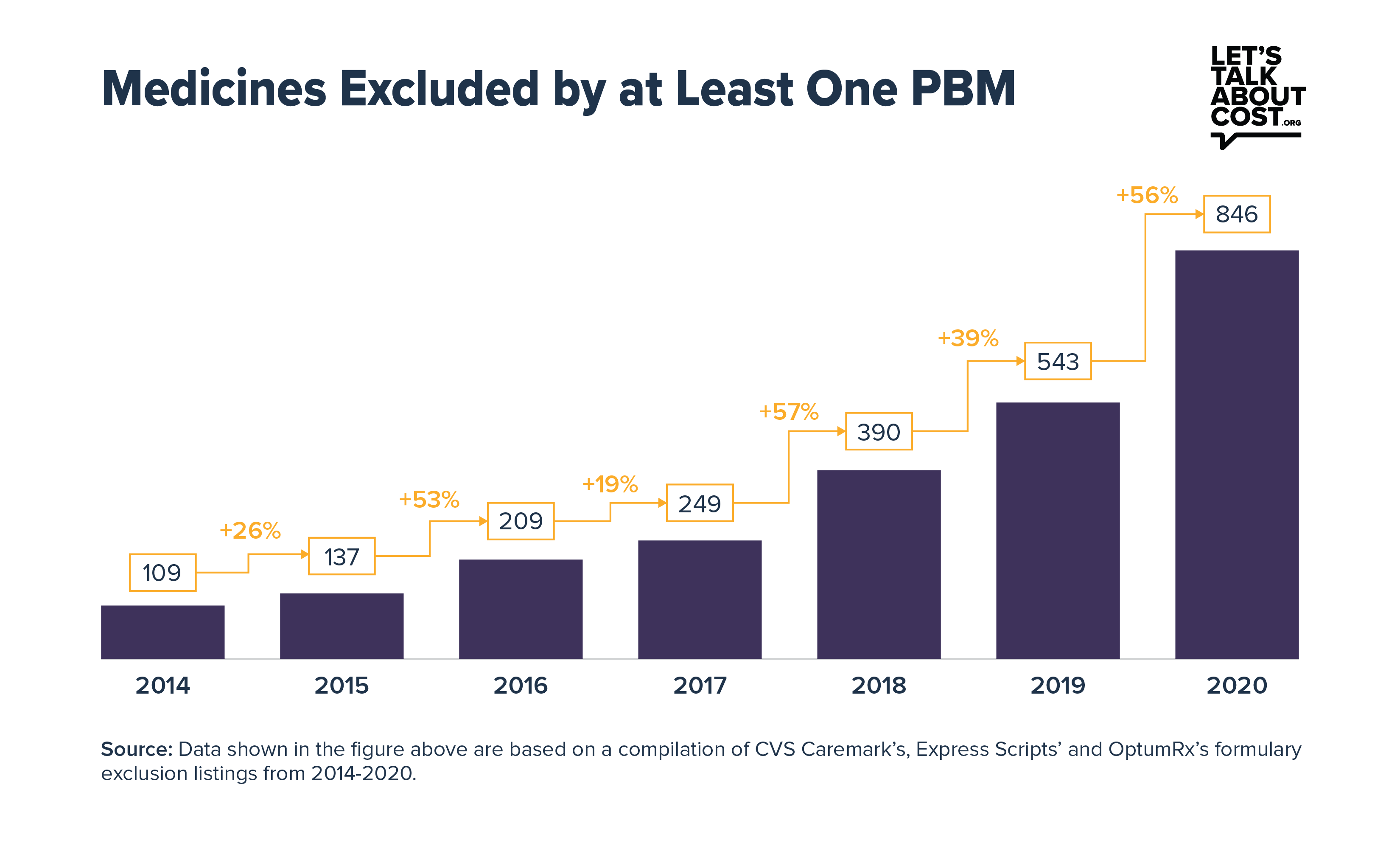
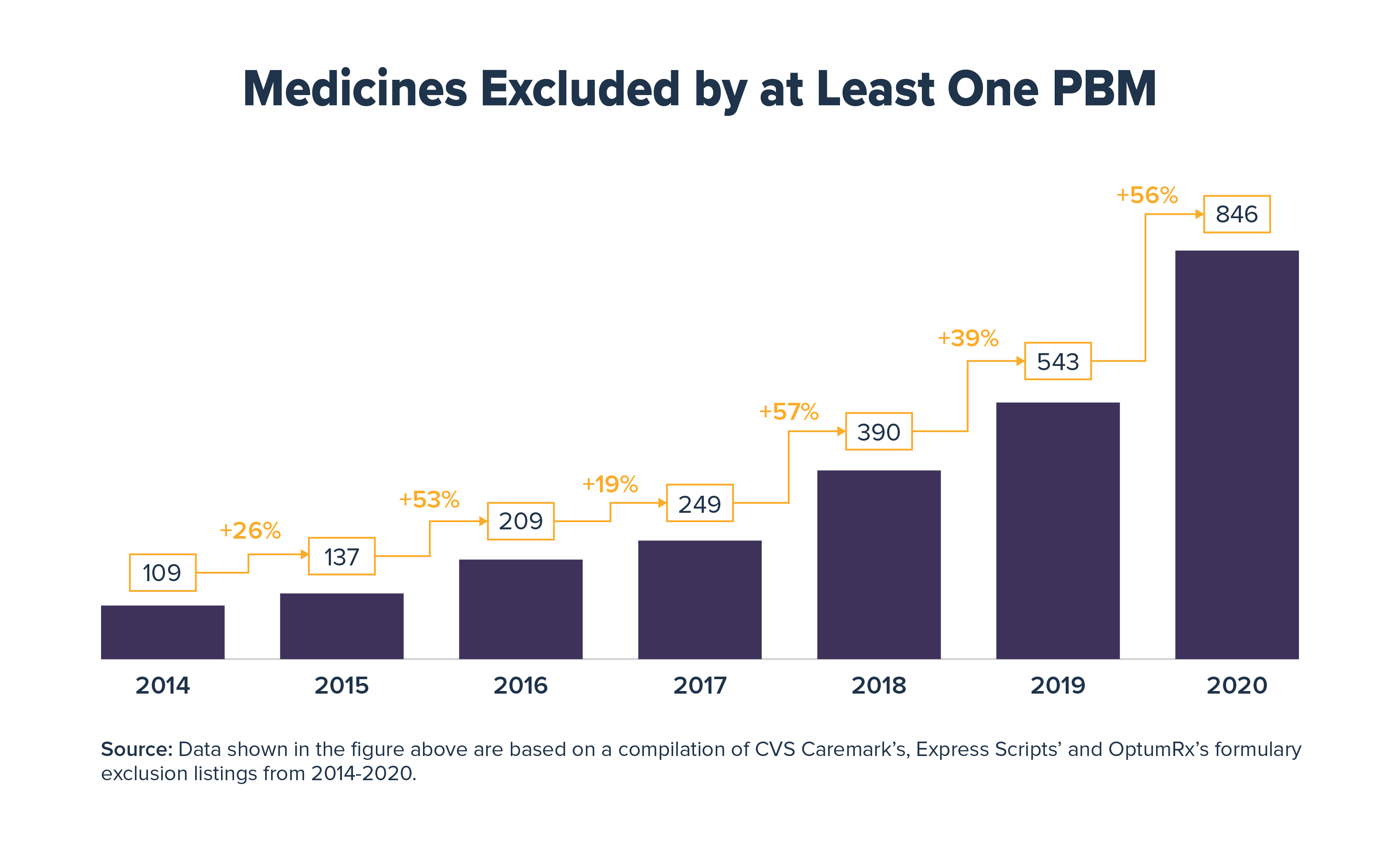
A new study from Xcenda finds that from 2014 to 2020, the number of medicines excluded by at least one of the three largest pharmacy benefit managers (PBMs) from their standard formularies increased by an average of 34% per year. As a result, each year hundreds of thousands of patients with commercial insurance may not be able to access the treatment prescribed by their doctor.
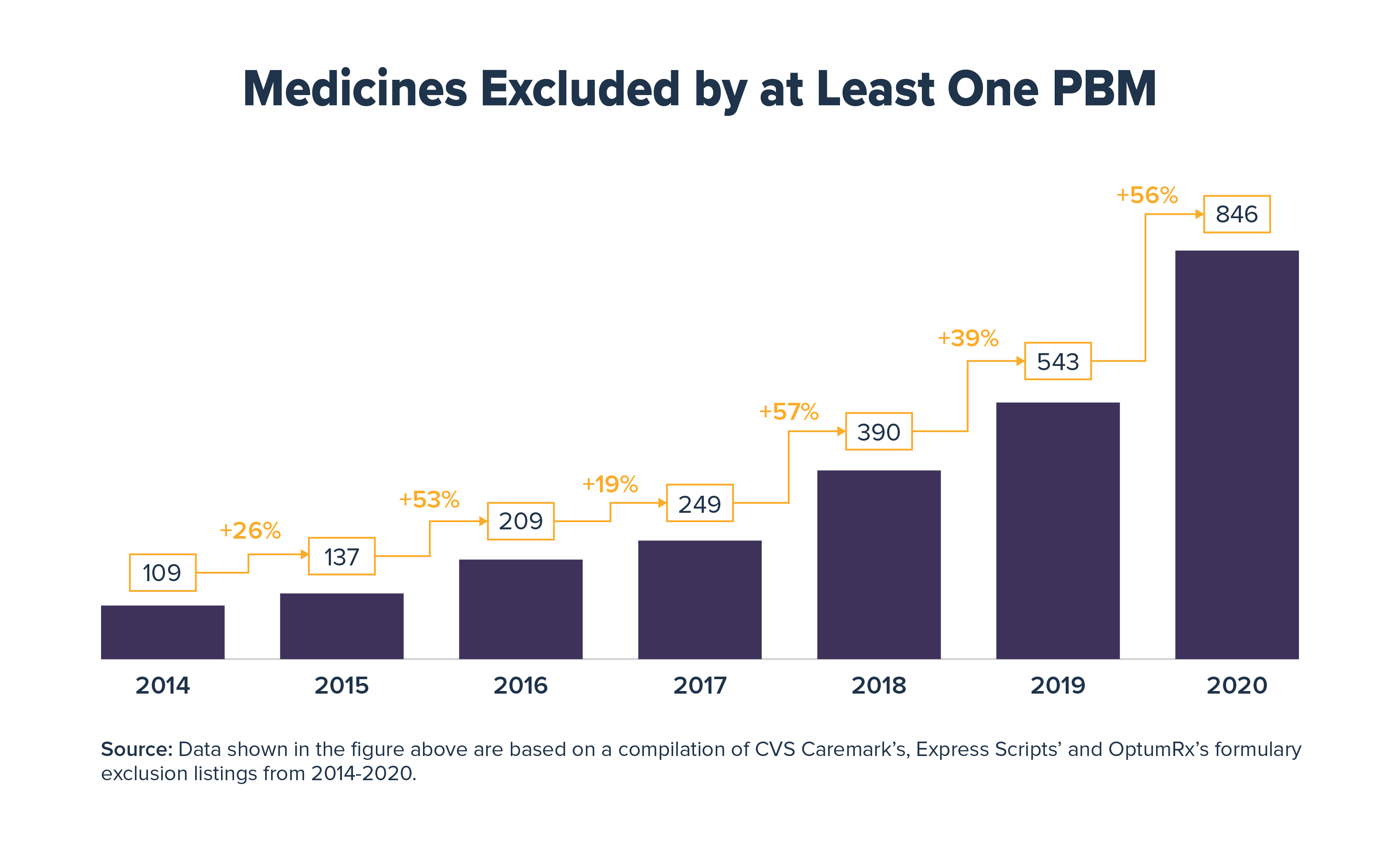
The study looked at the 2014 to 2020 formulary exclusion lists for Express Scripts, CVS Caremark and OptumRx, middlemen who collectively handle nearly three-quarters of all prescriptions in the United States. This year alone, 846 medicines were excluded from the standard commercial market formularies of at least one of these PBMs, up from 109 medicines in 2014. These formulary exclusions may affect patient adherence if they prevent or delay access to medicines, which can lead to adverse health outcomes.
The study also found:
- In 2020, 201 medicines were excluded from at least two PBM formularies and 74 were excluded from all three
- 20% of the medicines excluded from all three PBM formularies in 2020 were brand medicines without generic equivalents or biosimilar alternatives
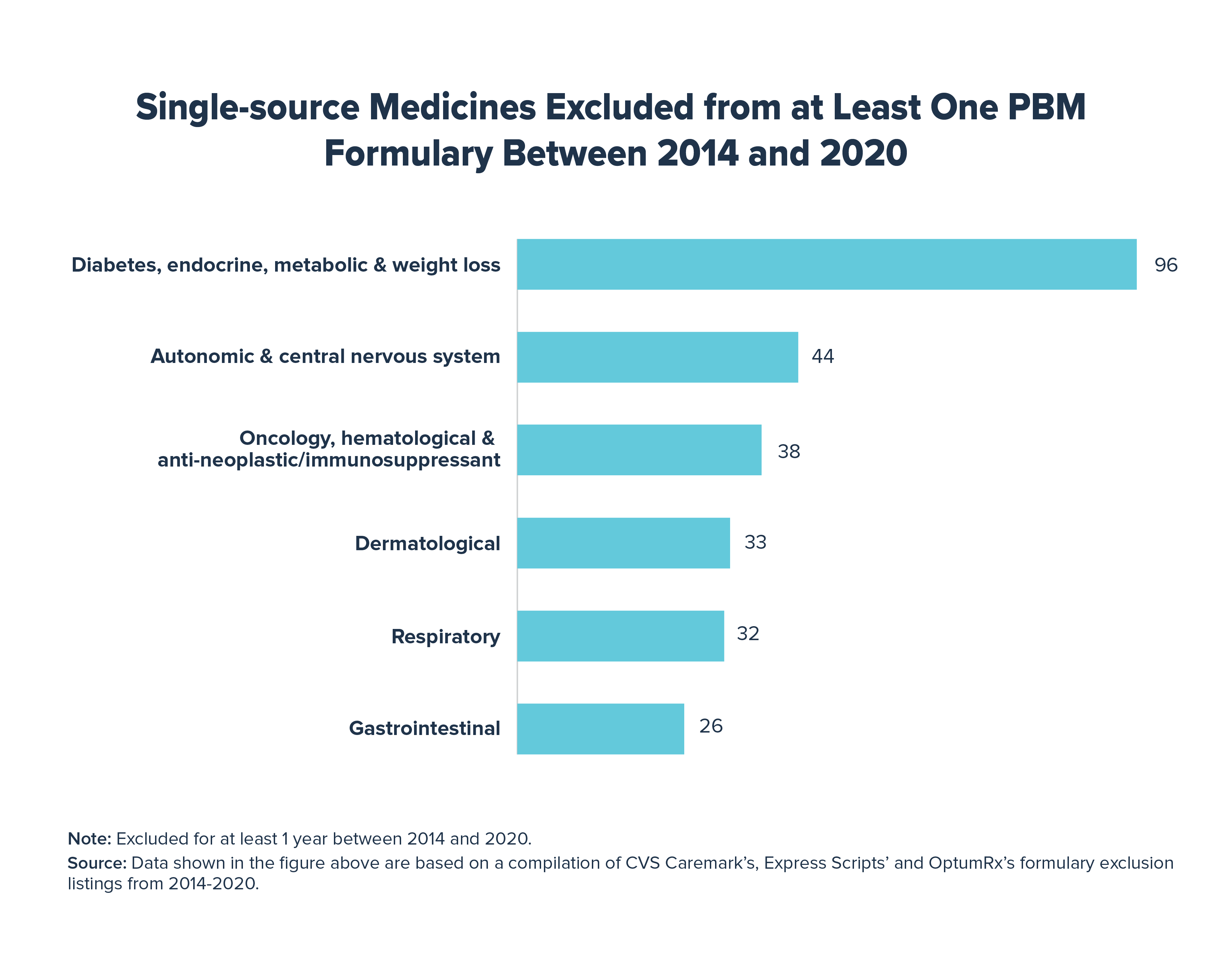
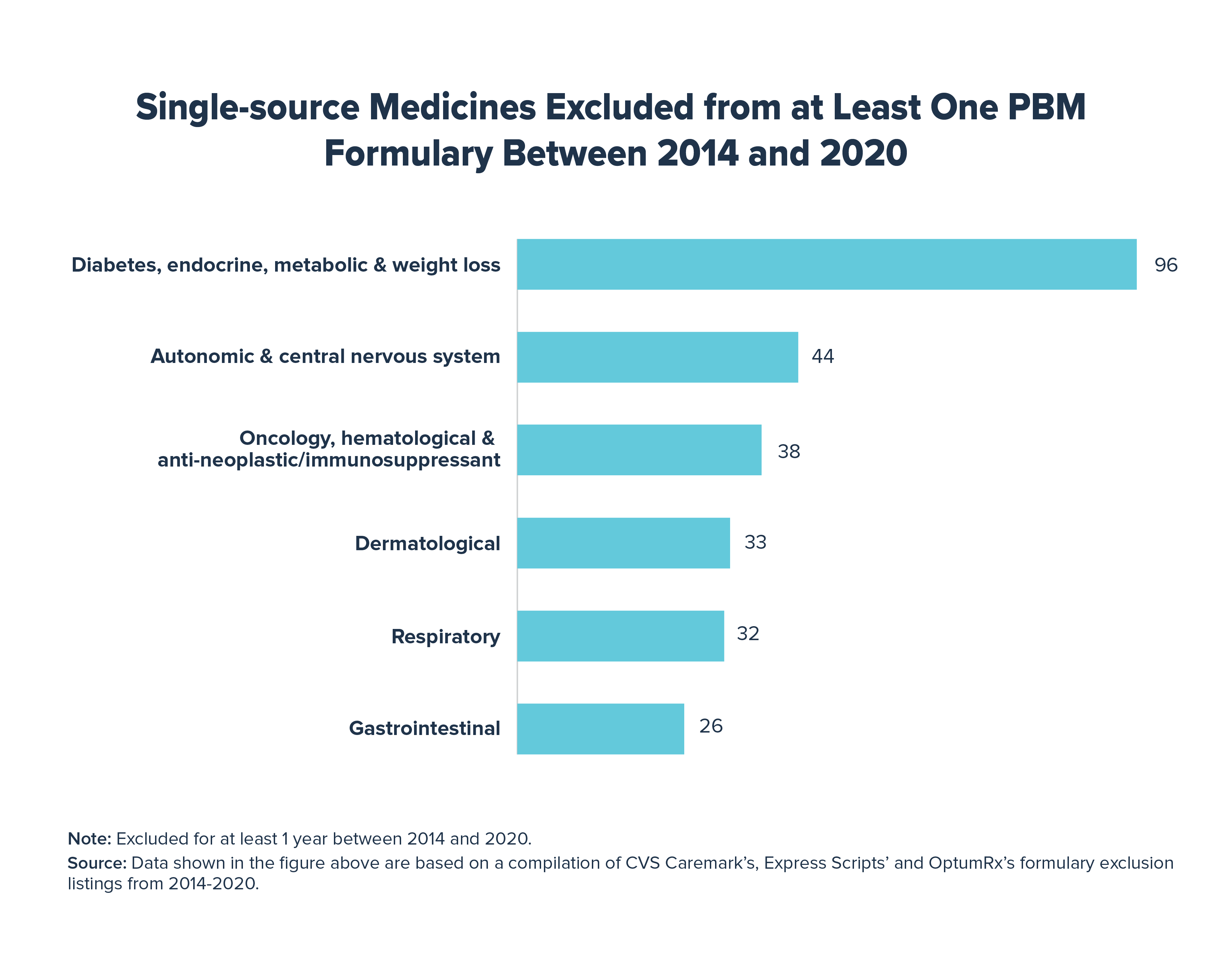
- Between 2014 and 2020, 943 medicines faced exclusion by one or more PBM for at least one year
- 2 of the 3 PBMs excluded lower price “authorized generic” versions of certain insulin and hepatitis C medicines, even though these exclusions could significantly increase out-of-pocket costs for patients with deductibles and coinsurance
- Medicines to treat chronic diseases, including insulin, antidepressants, antipsychotics, and antiarrhythmics, were most frequently targeted by formulary exclusions
Formulary exclusions may have an outsized impact on patients with chronic conditions, as they may develop resistance or experience diminishing results from medicines over time and may need to cycle through several treatments. While some patients who face exclusions for treatments prescribed by their physicians are able to petition for coverage, this time-consuming and burdensome process – for both patients and providers – could lead to delayed access to treatments.
Physicians, not middlemen, should make clinical determinations regarding which treatment is best for a patient. Allowing middlemen to insert themselves into the patient-physician decision-making process is not in the best interests of patients or the health care system. We have long advocated for policies to reform the role of middlemen in the health care system, including increasing PBM transparency with employers, sharing rebates directly with patients at the pharmacy counter and ending the practice of PBMs and other entities in the supply chain receiving fees based on a percentage of the price of a medicine.
View the study here and learn more at www.letstalkaboutcost.org.